ABSTRACT
Tumor necrosis factor (TNF) is an important mediator that triggers onset of autoimmune diseases and exerts its biological effects by interacting through two receptors, TNFR1 (also known as TNFRSF1A) and TNFR2 (also known as TNFRSF1B). TNFR2 signaling has significant potential to exert pro-survival and protective roles in several diseases. Unlike TNFR1 signaling, however, the mechanism of TNFR2 signal transduction is poorly understood, and few of its adaptor molecules are known. The present study utilized a proteomics approach to search for adaptor molecules in the TNFR2 signaling complex and identified aminopeptidase P3 (APP3, also known as XPNPEP3) to be a key molecule. One of its two isoforms, mitochondrial APP3 (APP3m) but not cytosolic APP3 (APP3c), was recruited to TNFR2 and shown to regulate TNF–TNFR2-dependent phosphorylation of JNK1 (also known as MAPK8) and JNK2 (also known as MAPK9). Furthermore, APP3m was released from mitochondria upon TNF stimulation in the absence of mitochondrial outer membrane permeabilization (MOMP). The observation of increased cell death upon downregulation of APP3m also suggested that APP3m exerts an anti-apoptotic function. These findings reveal that APP3m is a new member of the TNF–TNFR2 signaling complex and characterize an APP3-mediated TNFR2 signal transduction mechanism that induces activation of JNK1 and JNK2.
INTRODUCTION
Tumor necrosis factor (TNF) is a key signaling molecule in the immune system and is associated with pathogenesis, because it can exacerbate autoimmune diseases such as rheumatoid arthritis, inflammatory bowel disease and multiple sclerosis. TNF interacts with two receptors, TNF receptor type I (TNFR1, also known as TNFRSF1A) and TNF receptor type II (TNFR2, also known as TNFRSF1B). These receptors are expressed on different cell types and transmit cellular signals by distinct pathways (MacEwan, 2002), respectively. TNFR1 is constitutively expressed in most cell types, whereas TNFR2 is typically restricted to certain subpopulations of immune cells such as CD4+ or CD8+ T cells and a few other cell types such as oligodendrocytes and endothelial cells (Chan and Lenardo, 2000; Choi et al., 2005; Naudé et al., 2011; Cabal-Hierro and Lazo, 2012). Recent reports have clarified that some causes and exacerbations of disease are related to TNF receptor signaling, especially TNFR2. In the TNFΔARE mouse model of rheumatoid arthritis, in which the disease is attributed to overexpression of TNF, TNFR2 deficiency evokes aggravated arthritis and joint destruction as compared with wild-type mice (Kontoyiannis et al., 1999.). In addition, in the MOG35–55-induced experimental autoimmune encephalomyelitis (EAE) mouse model of the human demyelinating disease multiple sclerosis, TNFR2 deficiency exacerbates demyelination (Kontoyiannis et al., 1999; Suvannavejh et al., 2000). Furthermore, recent reports suggest that TNFR2 signaling also mediates myocardial protection (Monden et al., 2007; Wang et al., 2008), neuroprotection (Arnett et al., 2001; Fontaine et al., 2002) and activity of regulatory T cells (Treg) (Chen et al., 2007; Chen et al., 2010; Chen et al., 2013). Furthermore, the molecular mechanisms of signal initiation have been revealed through analysis of the X-ray crystal structure of the TNF–TNFR2 signaling complex (Mukai et al., 2010). Thus, these studies of TNFR2 suggest that there is an undeveloped potential of TNFR2 as a therapeutic target for autoimmune diseases (Faustman and Davis, 2010).
The binding of ligands to TNFR1 induces the formation of a receptor complex and subsequent activation of signaling pathways (Micheau and Tschopp, 2003). The intracellular region of TNFR1 has a death domain, and activation of downstream signals is mediated by the recruitment of several cytosolic proteins through this death domain. In addition to TNF-receptor-associated factors (TRAFs), two other families of death-domain-containing proteins (TRADD and FADD) have been described to date. TNFR1 signaling is controlled by these adaptor molecules both spatially and temporally, and these pathways regulate various physiological responses, notably proinflammatory responses and apoptosis (Chen and Goeddel, 2002; Micheau and Tschopp, 2003; Wajant et al., 2003). By contrast, TNFR2 lacks a death domain in its intracellular region, but it directly binds to and forms a complex with TRAF2 upon TNF stimulation, leading to the activation of nuclear factor κB (NF-κB) (Naudé et al., 2011; Cabal-Hierro and Lazo, 2012) and JNK (Al-Lamki et al., 2005; Matsuzawa et al., 2008). Thus, TNFR1 signaling mechanisms, which involve the functions of adaptor molecules, have been widely researched. However, the mechanism by which TNFR2 activates downstream signals is poorly defined. Therefore, we hypothesized that adaptor molecules other than TRAF2 might exist and tried to search for these proteins.
TNFR1 and TNFR2 interact closely with each other through crosstalk by sharing some adaptor molecules, such as TRAF2 (Naudé et al., 2011). This molecular crosstalk makes it complicated to elucidate the roles of each TNF receptor in cell proliferation and apoptosis. In order to activate TNFR2 specifically, a TNFR2-specific agonist (R2-7) was generated from a mutated TNF library using phage-display technology (Shibata et al., 2008; Nomura et al., 2009). By using this technology, R2-7 was identified as a TNFR2-selective TNF mutant protein with six amino acid mutations (positions at 29, 31, 32, 145, 146 and 147) from wild-type TNF (wtTNF). This agonist has a binding selectivity that is enhanced 180,000-fold but it retains a bioactivity that is comparable to wtTNF (Abe et al., 2011). Moreover, a HEK293T cell line that stably expresses TNFR2 has been established, allowing isolation of abundant ligand–receptor complexes. Previous studies have indicated that receptors that are expressed at a very low abundance, such as TNFR2, can be overexpressed in order to characterize the resulting enhanced amplification pathways. Thus, the TNFR2-expressing cell line can be used to analyze the molecular assemblies associated with TNFR2 signaling. Furthermore, highly sensitive proteomic analysis provides a powerful means to exhaustively detect proteins of very low abundance that form ligand–receptor complexes. This approach has been used to identify proteins associated with an affinity-purified TNF–TNFR2 signaling complex isolated from HEK293T cells.
The present study identifies aminopeptidase P3 (APP3, also known as XPNPEP3) as a member of the TNF–TNFR2 complex and demonstrates its role in this signaling pathway. It also reveals a new mechanism of JNK activation in TNFR2 signaling that is utilized by R2-7, a TNFR2-specific binding mutant of TNF.
RESULTS
Purification of the TNFR2 signaling complex
TNFR2, like TNFR1, forms a ligand–receptor complex to carry out signal transduction. Moreover, endogenous TRAF2 is recruited to TNFR2 in a ligand-dependent manner. In order to discover new adaptor molecules for TNFR2, we attempted to purify the TNFR2 signaling complex. Previous reports have used that the human kidney embryonic cell line HEK293T successfully in studies of TNFR adaptor proteins isolated after TNF stimulation (Kuai et al., 2003; Pincheira et al., 2008). TNFR1 was expressed on HEK293T cells, whereas TNFR2 was expressed only at a very low level (Fig. 1A). Previous reports have shown that an endogenous receptor complex can be affinity purified for FLAG-tagged ligand analysis (Kuai et al., 2003; Kuai et al., 2004). After stimulation of HEK293T cells with FLAG-tagged wild-type TNF (wtTNF–FLAG) or with the FLAG-tagged TNF mutant R2-7 (R2-7–FLAG), immunoprecipitation using anti-FLAG-antibody-conjugated beads (anti-FLAG immunoprecipitation) was performed (supplementary material Fig. S1A). TNFR1 and a small amount of TRAF2 were detected in the immunoprecipitate from wtTNF–FLAG-stimulated cells by western blotting, whereas TNFR2 was not detected in either wtTNF–FLAG or R2-7–FLAG-stimulated cells (Fig. 1B). These results indicate that the expression of TNFR2 is limited because it is not detected in the cell lysate.
Formation of a TNFR2 signaling complex in cells overexpressing TNFR2. (A) Expression of human TNFR1 and TNFR2 in HEK293T and HEK293T-TNFR2 cells was analyzed by flow cytometry. Cells stained by a biotinylated anti-TNFR1 or anti-TNFR2 antibody are indicated by the black line histogram. Cells stained with an isotype control antibody and unstained cells are shown by the dotted line and gray-filled histograms, respectively. (B) Formation of the TNFR2 signaling complex in HEK293T and HEK293T-TNFR2 cells was analyzed. Cells were stimulated with TNF–FLAG (100 ng/ml) or R2-7–FLAG (100 ng/ml) for 30 minutes. After cell lysis, the TNFR2 signaling complex was recovered by anti-FLAG immunoprecipitation (IP). Untreated cells were analyzed in the same way. The cell lysate and immunoprecipitate were analyzed by western blotting (IB) with anti-TNF, anti-TNFR1, anti-TNFR2 or anti-TRAF2 antibody.
Formation of a TNFR2 signaling complex in cells overexpressing TNFR2. (A) Expression of human TNFR1 and TNFR2 in HEK293T and HEK293T-TNFR2 cells was analyzed by flow cytometry. Cells stained by a biotinylated anti-TNFR1 or anti-TNFR2 antibody are indicated by the black line histogram. Cells stained with an isotype control antibody and unstained cells are shown by the dotted line and gray-filled histograms, respectively. (B) Formation of the TNFR2 signaling complex in HEK293T and HEK293T-TNFR2 cells was analyzed. Cells were stimulated with TNF–FLAG (100 ng/ml) or R2-7–FLAG (100 ng/ml) for 30 minutes. After cell lysis, the TNFR2 signaling complex was recovered by anti-FLAG immunoprecipitation (IP). Untreated cells were analyzed in the same way. The cell lysate and immunoprecipitate were analyzed by western blotting (IB) with anti-TNF, anti-TNFR1, anti-TNFR2 or anti-TRAF2 antibody.
Therefore, an alternative approach was adopted to establish a cell line that stably overexpressed TNFR2 in order to recover the TNFR2 complex. The human TNFR2 gene was transfected into HEK293T cells, and TNFR2-positive cells were collected using a cell sorter. The TNFR1 expression level of the TNFR2-expressing HEK293T (HEK293T-TNFR2) cells was almost equal to that of the parental HEK293T cells, but the TNFR2 expression level was significantly increased (Fig. 1A). After stimulating HEK293T-TNFR2 cells with wtTNF–FLAG and R2-7–FLAG, anti-FLAG immunoprecipitation was performed. Both TNFR1 and TNFR2 were detected by immunoprecipitation in wtTNF–FLAG stimulated cells, but only TNFR2 was detected in R2-7–FLAG stimulated cells (Fig. 1B). Furthermore, TRAF2 was detected after either wtTNF–FLAG or R2-7–FLAG stimulation. The TNFR2 complex including APP3 did not form incidentally in unstimulated HEK293T-TNFR2 cell lysate after the addition of ligand, even though TNF and TNFR2 interacted with each other in cell lysate (supplementary material Fig. S2); therefore, it formed in a manner dependent on ligand stimulation. Thus, R2-7–FLAG stimulation followed by anti-FLAG immunoprecipitation was able to specifically recover a TNFR2 complex.
Identification of adaptor proteins included in the TNFR2 signaling complex
In order to identify new adaptor molecules of TNFR2, the complex was analyzed using a proteomic approach. Binding of the TNF homotrimer to TNFR2 induces aggregation of the receptors and subsequent recruitment of cytosolic signaling proteins, resulting in the formation of a ligand–TNFR2 complex that initiates downstream signal transduction. Therefore, purification of these proteins is important for identifying signal-related proteins or transcription factors that are expressed at low levels. R2-7–FLAG promoted formation of the TNFR2 complex specifically, and subsequent affinity purification by anti-FLAG immunoprecipitation enabled us to concentrate the target proteins. These precipitates were analyzed by liquid chromatography mass spectrometry (LC-MS) after tryptic digestion. A MASCOT database search indicated that ∼600 and 570 proteins were identified with and without R2-7–FLAG stimulation, respectively (supplementary material Tables S1 and S2).
Comparative analysis of results obtained for stimulated versus unstimulated cells indicated that 142 proteins were specifically detected in the stimulated cells. These proteins were therefore considered to be potential TNFR2-signaling-related proteins. Among these, proteins with a protein score over 100, which we applied as a selection criterion, were considered as candidates as adaptor molecules (Fig. 2A). The protein score is based on the number of peptides matching the protein in the database and the accuracy of those matches: higher protein scores indicate higher degrees of match. TNFR2 and TRAF2 were identified as having top scores and coverage. Baculoviral IAP repeat-containing protein 2 (cIAP1), which is known to be a TNFR2 adaptor molecule, was also detected. These results verified that R2-7-stimulated TNFR2 formed a receptor complex with TRAF2 and cIAP1 protein.
Identification of a new TNFR2 adaptor protein. (A) High scoring proteins (Protein score >100) identified in the R2-7–TNFR2 complex by mass spectrometry analysis are listed. These proteins were detected only in R2-7–FLAG-treated cells and not in untreated cells. Proteins are listed in descending order of protein score. ‘Accession’ is the identifier used for UniProt; ‘Protein score’ is the identification score obtained with Mascot software; ‘Coverage’ is the percentage of sequence coverage obtained with identified peptides; ‘Number of peptides’ is the number of experimentally obtained peptides matching theoretical peptides in the database; ‘Mr’ is the theoretical molecular masses of the proteins. Proteins indicated in bold are known to be included in the TNFR2 signaling complex. (B) HEK293T and HEK293T-TNFR2 cells were stimulated with TNF–FLAG (100 ng/ml) or R2-7–FLAG (100 ng/ml) for 30 minutes. After cell lysis, the TNFR2 signaling complex was recovered by anti-FLAG immunoprecipitation (IP). The immunoprecipitates were assessed by western blotting (IB) with anti-APP3, anti-cIAP1, anti-HTRA2 or anti-DIABLO antibody. (C) Expression of transiently expressed human TNFR1 on HEK293T cells was analyzed by flow cytometry. TNFR1 expression on parental HEK293T and HEK293T-TNFR1 cells is indicated by a dotted line and solid line, respectively. Unstained HEK293T cells are shown by the gray-filled histogram. + and +++ indicate the relative expression level of TNFR1 on each cell. (D) Recruitment of APP3 to TNFR1 by TNF stimulation was analyzed in human HEK293T cells transiently expressing TNFR1. HEK293T (TNFR1+) cells and HEK293T-TNFR1 (TNFR1+++) were stimulated with TNF–FLAG (100 ng/ml) for 30 minutes. After cell lysis, interaction of TNFR1 and APP3 was confirmed by immunoprecipitation followed by western blotting.
Identification of a new TNFR2 adaptor protein. (A) High scoring proteins (Protein score >100) identified in the R2-7–TNFR2 complex by mass spectrometry analysis are listed. These proteins were detected only in R2-7–FLAG-treated cells and not in untreated cells. Proteins are listed in descending order of protein score. ‘Accession’ is the identifier used for UniProt; ‘Protein score’ is the identification score obtained with Mascot software; ‘Coverage’ is the percentage of sequence coverage obtained with identified peptides; ‘Number of peptides’ is the number of experimentally obtained peptides matching theoretical peptides in the database; ‘Mr’ is the theoretical molecular masses of the proteins. Proteins indicated in bold are known to be included in the TNFR2 signaling complex. (B) HEK293T and HEK293T-TNFR2 cells were stimulated with TNF–FLAG (100 ng/ml) or R2-7–FLAG (100 ng/ml) for 30 minutes. After cell lysis, the TNFR2 signaling complex was recovered by anti-FLAG immunoprecipitation (IP). The immunoprecipitates were assessed by western blotting (IB) with anti-APP3, anti-cIAP1, anti-HTRA2 or anti-DIABLO antibody. (C) Expression of transiently expressed human TNFR1 on HEK293T cells was analyzed by flow cytometry. TNFR1 expression on parental HEK293T and HEK293T-TNFR1 cells is indicated by a dotted line and solid line, respectively. Unstained HEK293T cells are shown by the gray-filled histogram. + and +++ indicate the relative expression level of TNFR1 on each cell. (D) Recruitment of APP3 to TNFR1 by TNF stimulation was analyzed in human HEK293T cells transiently expressing TNFR1. HEK293T (TNFR1+) cells and HEK293T-TNFR1 (TNFR1+++) were stimulated with TNF–FLAG (100 ng/ml) for 30 minutes. After cell lysis, interaction of TNFR1 and APP3 was confirmed by immunoprecipitation followed by western blotting.
Among the proteins identified by proteomics, proteins that appeared to be unrelated to signal transduction, such as membrane proteins or ribosomal proteins, were excluded. Of these proteins we found that APP3 showed the highest protein score and coverage after TNFR2 and TRAF2. In addition, the mitochondrial serine protease HTRA2 and a mitochondrial Diablo homolog (DIABLO), which are pro-apoptotic proteins released from mitochondria, were identified. These proteins are known to inhibit the suppression of caspase by interacting with cIAP proteins in TNFR1 signaling (Verhagen et al., 2000). However, it is unclear whether these proteins bind to TNFR2 from previous studies. Therefore, we performed anti-FLAG immunoprecipitation to examine the binding activity of APP3, cIAP1, HTRA2 and DIABLO against TNFR2 (Fig. 2B). The detection of APP3 and cIAP1 was ligand dependent by western blotting analysis; by contrast, DIABLO and HTRA2 were also detected in the untreated group. DIABLO and HTRA2 seem more likely to be recovered nonspecifically by anti-FLAG immunoprecipitation without ligand stimulation. As indicated above, however, DIABLO and HTRA2 are well-known as cIAP-binding proteins; thus, the possibility that they bind TNFR2 through cIAP1 remains. Hence, APP3 was determined as a new adaptor protein of TNFR2. Furthermore, to exclude effect of TNFR1 expression level, recruitment of APP3 was confirmed in HEK293T cells transiently expressing TNFR1 (HEK293T-TNFR1) (Fig. 2C). Regarding the results of anti-FLAG immunoprecipitation, APP3 was below the detection limit in HEK293T-TNFR1 cells (Fig. 2D). Even when the TNFR1 expression was increased, the amount of APP3 binding did not change. These results indicate that APP3 binds to TNFR2 specifically. Therefore, we focused on the potential role of APP3 in TNFR2 signaling, and proceeded to analyze the functions of this molecule.
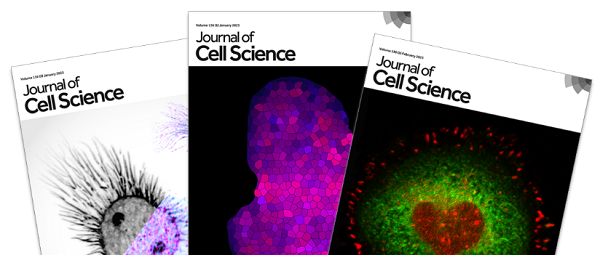
Mitochondrial APP3 binds to TNFR2
A previous report has shown that APP3 has two isoforms, a mitochondrial isoform APP3m (57 kDa) and a cytoplasmic isoform APP3c (48 kDa), which are owing to alternative splicing (Erşahin et al., 2005). APP3m has an N-terminal mitochondrial-targeting sequence (MTS) domain that leads to its import into mitochondria (Fig. 3A). APP3m functions as a 51-kDa mature protein after the MTS is removed proteolytically in mitochondria. By contrast, APP3c, lacks the MTS and is expressed in the cytosol. Indeed, APP3m and APP3c were detected as different sized molecules in the cell lysate of HEK293T-TNFR2 (Fig. 3B). It is known that the mutation of arginine residues to alanine residues in the MTS prevents distribution in mitochondria because arginine is required for mitochondrial transport (Goto et al., 2009; Whatcott et al., 2009). To confirm whether the MTS is actually removed, APP3m, APP3c and an APP3m MTS mutant (APP3m MTSΔR, in which Arg18, Arg29, Arg30, Arg39, Arg40, and Arg44 of MTS were replaced with alanine residues) were overexpressed in the cell, and the molecular mass of each protein was compared by western blotting. We found that APP3m MTSΔR, although its expression level was low, was detected as a 57-kDa protein of different size from APP3m and APP3c. Therefore, APP3m is mostly present as the 51-kDa mature protein after MTS removal following import into mitochondria.
Recruitment of APP3m but not APP3c to TNF–TNFR2 complex. (A) APP3 has two differentially localized isoforms. APP3m (57 kDa) has an N-terminal mitochondrial-targeting sequence (MTS) domain, and is imported into mitochondria where it localizes as a 51-kDa mature enzyme. APP3c (48 kDa), lacking MTS, is expressed in the cytosol. An NCBI search for conserved domains predicted an aminopeptidase P, N-terminal domain (AMP_N) and prolidase domain in each APP3. (B) In HEK293T-TNFR2 cells, transiently expressing APP3m and APP3c were detected as 51-kDa and 48-kDa proteins, respectively, as described in A. APP3m in which arginine residues are replaced with alanine residues in the MTS domain (APP3m MTSΔR), was expressed as a protein of ∼57 kDa, although its expression level was low. APP3m was mostly present as the 51-kDa protein in APP3m-transfected cells. (C) HEK293T-TNFR2 cells that transiently expressed APP3m–HA or APP3c–HA were stimulated with TNF (100 ng/ml) or R2-7 (100 ng/ml) for 30 minutes. Anti-HA immunoprecipitation (IP) showed that R2-7, as well as TNF, recruited APP3m to TNFR2, but APP3c was not recruited. (D) Anti-FLAG immunoprecipitation was performed using APP3-transfected HEK293T-TNFR2 after R2-7–FLAG (100 ng/ml) stimulation. Western blotting confirmed that endogenous APP3m was detected in cells transfected with both APP3m–HA and APP3c–HA. However, transfected APP3 was detected only in the APP3m–HA transfectant with anti-HA antibody. (E) Aminopeptidase P activity was measured in anti-FLAG immunoprecipitates. Only elutes from cells transfected with APP3m–HA, and not APP3c–HA, showed higher enzymatic activity. Results are mean±s.d., n = 3. **P<0.01 (Student's t-test). (F) APP3m–HA mutants, in which the MTS domain 1–45 [APP3m MTSΔ(1–45)–HA] or 1–53 [APP3m MTSΔ(1–53)–HA] was deleted, were expressed in cells. After R2-7 (100 ng/ml) stimulation for 30 min, anti-HA immunoprecipitation was performed. Western blotting showed that these mutants bound to TNFR2 as indicated in the schematic in the right-hand panel, and that a 26-amino-acid sequence (shaded region in the schematic) was essential for TNFR2 binding. (G) HEK293T-TNFR2 cells were treated with R2-7–FLAG (100 ng/ml) for the indicated time. After cell lysis, to confirm time-dependent recruitment of APP3 to the receptor, anti-FLAG immunoprecipitation was performed followed by western blotting. (H) HA-tagged APP3m (APP3m–HA) or APP3c-HA was transiently expressed in HEK293T-TNFR2 cells. R2-7 (100 ng/ml) stimulation followed by anti-HA immunoprecipitation was performed to determine the time-dependent manner of APP3m or APP3c recruitment to the TNFR2 signaling complex. Western analysis was performed with anti-APP3, anti-TNFR2 or anti-TRAF2 antibody.
Recruitment of APP3m but not APP3c to TNF–TNFR2 complex. (A) APP3 has two differentially localized isoforms. APP3m (57 kDa) has an N-terminal mitochondrial-targeting sequence (MTS) domain, and is imported into mitochondria where it localizes as a 51-kDa mature enzyme. APP3c (48 kDa), lacking MTS, is expressed in the cytosol. An NCBI search for conserved domains predicted an aminopeptidase P, N-terminal domain (AMP_N) and prolidase domain in each APP3. (B) In HEK293T-TNFR2 cells, transiently expressing APP3m and APP3c were detected as 51-kDa and 48-kDa proteins, respectively, as described in A. APP3m in which arginine residues are replaced with alanine residues in the MTS domain (APP3m MTSΔR), was expressed as a protein of ∼57 kDa, although its expression level was low. APP3m was mostly present as the 51-kDa protein in APP3m-transfected cells. (C) HEK293T-TNFR2 cells that transiently expressed APP3m–HA or APP3c–HA were stimulated with TNF (100 ng/ml) or R2-7 (100 ng/ml) for 30 minutes. Anti-HA immunoprecipitation (IP) showed that R2-7, as well as TNF, recruited APP3m to TNFR2, but APP3c was not recruited. (D) Anti-FLAG immunoprecipitation was performed using APP3-transfected HEK293T-TNFR2 after R2-7–FLAG (100 ng/ml) stimulation. Western blotting confirmed that endogenous APP3m was detected in cells transfected with both APP3m–HA and APP3c–HA. However, transfected APP3 was detected only in the APP3m–HA transfectant with anti-HA antibody. (E) Aminopeptidase P activity was measured in anti-FLAG immunoprecipitates. Only elutes from cells transfected with APP3m–HA, and not APP3c–HA, showed higher enzymatic activity. Results are mean±s.d., n = 3. **P<0.01 (Student's t-test). (F) APP3m–HA mutants, in which the MTS domain 1–45 [APP3m MTSΔ(1–45)–HA] or 1–53 [APP3m MTSΔ(1–53)–HA] was deleted, were expressed in cells. After R2-7 (100 ng/ml) stimulation for 30 min, anti-HA immunoprecipitation was performed. Western blotting showed that these mutants bound to TNFR2 as indicated in the schematic in the right-hand panel, and that a 26-amino-acid sequence (shaded region in the schematic) was essential for TNFR2 binding. (G) HEK293T-TNFR2 cells were treated with R2-7–FLAG (100 ng/ml) for the indicated time. After cell lysis, to confirm time-dependent recruitment of APP3 to the receptor, anti-FLAG immunoprecipitation was performed followed by western blotting. (H) HA-tagged APP3m (APP3m–HA) or APP3c-HA was transiently expressed in HEK293T-TNFR2 cells. R2-7 (100 ng/ml) stimulation followed by anti-HA immunoprecipitation was performed to determine the time-dependent manner of APP3m or APP3c recruitment to the TNFR2 signaling complex. Western analysis was performed with anti-APP3, anti-TNFR2 or anti-TRAF2 antibody.
APP3m and APP3c have identical amino acid sequences except for an N-terminal extension of 79 amino acids on APP3m, as shown in Fig. 3A. MS/MS analysis detected only the identical region, but not any peptides derived from the N-terminal APP3m extension (data not shown); thus, it was not possible to determine which isoform was bound to TNFR2. Therefore, we used an alternative approach to determine which APP3 isoform binds to TNFR2. Immunoprecipitation with an anti-HA antibody (anti-HA immunoprecipitation) after TNF–FLAG or R2-7–FLAG stimulation was performed using cell lysates prepared from HEK293T-TNFR2 cells overexpressing HA-tagged APP3m (APP3m–HA) or APP3c (APP3c–HA) (supplementary material Fig. S1B). The western blot of the immunoprecipitate showed that TNFR2 was detected only in the cells that overexpressed APP3m–HA (Fig. 3C). Therefore, these results reveal that APP3m, but not APP3c, bound to TNFR2. The fact that APP3m bound to TNFR2 only upon receptor activation, and not as a steady-state interaction, indicates that APP3m is recruited to TNFR2 as an adaptor molecule during TNFR2 activation. Furthermore, the results of anti-FLAG immunoprecipitation from the same APP3-overexpressing cell lysates indicated that only overexpressed APP3m with protease activity bound to TNFR2, along with endogenous APP3m (Fig. 3D,E).
A previous study have shown that the MitoProt II program can predict processing sites in mitochondria (Erşahin et al., 2005). According to that report, APP3m is cleaved after an Arg-Xaa sequence by a mitochondrial processing peptidase (MPP), followed by the removal of N-terminal octapeptides by a mitochondrial intermediate peptidase (MIP). The MPP and MIP processing sites are located between Tyr45 and Leu46, and Thr53 and His54, respectively. To confirm the ability of APP3 to bind to TNFR2, two APP3m MTS deletion mutants, in which each of the potential processing sequences was deleted (APP3m MTSΔ1–45 and APP3m MTSΔ1–53, respectively), were overexpressed in HEK293T-TNFR2 cells along with APP3m and APP3c. We found that both APP3m MTSΔ1–45 and APP3m MTSΔ1–53 bound to TNFR2 to the same extent as APP3m (Fig. 3F). This result demonstrated that the region from His54 to Leu79 is essential for association with TNFR2.
It is known that TRAF2 binds to TNFR2 directly through interaction with the TRAF-C domain (Bradley and Pober, 2001) and TRAF2 also binds to TNFR2 in a time-dependent manner (Fischer et al., 2011b). Therefore, we examined whether APP3 bound to TNFR2 in the same manner as TRAF2 (Fig. 3G). R2-7–FLAG stimulation, followed by anti-FLAG immunoprecipitation revealed that APP3 bound to TNFR2 as well as to TRAF2. Recruitment of APP3 and TRAF2 was evoked after 3 minutes of stimulation, and the binding amount of APP3 remained constant, whereas that of TRAF2 decreased gradually. If APP3 binds to TNFR2 through TRAF2, then the amount of APP3 would be expected to decrease concomitantly with that of TRAF2. The observed discrepancy in the binding capacity of these proteins to this receptor suggests that APP3 and TRAF2 bind to TNFR2 independently. Furthermore, time-dependent recruitment of APP3m, but not APP3c, to TNFR2 was revealed by anti-HA immunoprecipitation of APP3-transfected cells (Fig. 3H). These results suggest that the active protease APP3m might be an important adaptor molecule in TNFR2 signaling.
APP3m translocates from mitochondria to the cytosol upon TNF stimulation
Because APP3m is normally located in mitochondria, it would be expected to translocate from mitochondria to the cytoplasm after TNFR2 activation. It is known that mitochondrial proteins such as cytochrome c, HTRA2 and DIABLO are released from the mitochondrial inter-membrane space (IMS) to the cytoplasm, in the induction of apoptosis mediated by TNFR1 signaling (Verhagen et al., 2000; van Loo et al., 2002; Schütze et al., 2008). To assess the recruitment of APP3m, we examined mitochondrial outer membrane permeabilization (MOMP) by a tetramethylrhodamine ethyl ester (TMRE) assay (Goldstein et al., 2005; Tait and Green, 2010). TMRE fluorescence, which was observed using a fluorescence microscope, was visible for 30 minutes after treatment with TNF or R2-7 in both HEK293T and HEK293T-TNFR2 cells (Fig. 4A). Carbonyl cyanide p-trifluoromethoxyphenylhydrazone (FCCP), which is a depolarizes the plasma membrane potential, substantially dispersed TMRE fluorescence in both cells. A similar result was obtained in a fluorescence microplate assay (Fig. 4B). These results indicate that MOMP did not occur in either HEK293T or HEK293T-TNFR2 cells until 30 minutes after stimulation.
Integrity of the mitochondrial outer membrane and localization of mitochondrial proteins. (A) HEK293T and HEK293T-TNFR2 cells were stained with 100 nM TMRE after treatment with TNF (100 ng/ml) or R2-7 (100 ng/ml). TMRE staining of mitochondria in live cells was measured by fluorescence microscopy (left panels). Brightfield microscopy coincided with fluorescence microscopy (right panels). FCCP (20 µM) was used as a positive control of mitochondrial membrane depolarization. (B) HEK293T and HEK293T-TNFR2 cells were stained with 500 nM TMRE after stimulation with TNF (100 ng/ml) or R2-7 (100 ng/ml) in a 96-well assay plate. TMRE staining of cells was also measured by a fluorescence plate reader. Results are mean±s.d., n = 3. (C) Subcellular fractionation was performed on HEK293T and HEK293T-TNFR2 cells. Localization of the major mitochondrial proteins was confirmed by western blotting. C, cytosolic fraction; M, mitochondrial fraction.
Integrity of the mitochondrial outer membrane and localization of mitochondrial proteins. (A) HEK293T and HEK293T-TNFR2 cells were stained with 100 nM TMRE after treatment with TNF (100 ng/ml) or R2-7 (100 ng/ml). TMRE staining of mitochondria in live cells was measured by fluorescence microscopy (left panels). Brightfield microscopy coincided with fluorescence microscopy (right panels). FCCP (20 µM) was used as a positive control of mitochondrial membrane depolarization. (B) HEK293T and HEK293T-TNFR2 cells were stained with 500 nM TMRE after stimulation with TNF (100 ng/ml) or R2-7 (100 ng/ml) in a 96-well assay plate. TMRE staining of cells was also measured by a fluorescence plate reader. Results are mean±s.d., n = 3. (C) Subcellular fractionation was performed on HEK293T and HEK293T-TNFR2 cells. Localization of the major mitochondrial proteins was confirmed by western blotting. C, cytosolic fraction; M, mitochondrial fraction.
Furthermore, we performed subcellular fractionation to confirm the mitochondrial localization of APP3m along with other mitochondrial proteins. APP3m was mainly detected in the mitochondrial fraction along with cytochrome c in both HEK293T and HEK293T-TNFR2 cells (Fig. 4C). HTRA2 and DIABLO are compartmentalized in mitochondria, where the apoptosis signal was not induced. Interestingly, however, these proteins were detected in the cytosol under the conditions used in our experiment. By contrast, the voltage-dependent anion channel (VDAC) and cytochrome c oxidase subunit IV (COX IV), which are present in the mitochondrial membrane, were detected in the mitochondrial fraction. Therefore, it is likely that the signaling mechanism of APP3 differs from that of HTRA2 and DIABLO because APP3m interacted with TNFR2 after R2-7 stimulation in the absence of MOMP.
There was no significant time-dependent alteration in the expression of either APP3 isoform after TNFR2 stimulation (Fig. 5A); therefore, we examined the kinetics of APP3m and APP3c qualitatively and quantitatively, in order to clarify the changes in their subcellular localization. We observed an alteration in the subcellular localization of APP3 and APP3c after treatment with R2-7. APP3m–Venus localized mostly in mitochondria in unstimulated cells, but it translocated to the cytoplasm after TNFR2 stimulation (Fig. 5B). By contrast, APP3c–Venus did not change its localization in the cytoplasm. Furthermore, APP3m and APP3c were detected in the cytoplasmic fraction after TNFR2 stimulation, whereas only APP3m was detected in the mitochondrial fraction by semi-quantitative analysis with western blotting (Fig. 5C).
Intracellular translocation of APP3m and APP3c by TNFR2 stimulation. (A) HEK293T-TNFR2 cells were stimulated with R2-7 (100 ng/ml) for the indicated time. After cell lysis, APP3m and APP3c were detected by western blotting. Representative images from three independent experiments are shown. The total intensity of both APP3 bands was determined by densitometric measurement. (B) HEK293T-TNFR2 cells transiently expressing APP3m–Venus and APP3c–Venus were stained with 200 nM MitoTracker Red CMXRos. The cells were then cultured with or without R2-7 (100 ng/ml) for 10 or 30 minutes, and fixed with 4% PFA. Nuclei were stained with DAPI. Localization of APP3m and APP3c was visualized using a confocal laser microscope. (C) HEK293T-TNFR2 cells were cultured with or without R2-7 (100 ng/ml) for 10 or 30 minutes. Recovered cells were separated into cytosolic and mitochondrial fractions by differential centrifugation. APP3m and APP3c detected by western blotting in each fraction were quantified by densitometric measurement of bands. Images from three independent experiments are shown. Results are mean±s.d., n = 3. **P<0.01 (Student's t-test). (D) APP3 enzymatic activity (mean±s.d.) in the cytosolic (squares) and mitochondrial fractions (triangles) was measured using a fluorescence assay after stimulation with or without R2-7 (100 ng/ml). *P<0.05, **P<0.01 (Student's t-test) compared with the unstimulated control group.
Intracellular translocation of APP3m and APP3c by TNFR2 stimulation. (A) HEK293T-TNFR2 cells were stimulated with R2-7 (100 ng/ml) for the indicated time. After cell lysis, APP3m and APP3c were detected by western blotting. Representative images from three independent experiments are shown. The total intensity of both APP3 bands was determined by densitometric measurement. (B) HEK293T-TNFR2 cells transiently expressing APP3m–Venus and APP3c–Venus were stained with 200 nM MitoTracker Red CMXRos. The cells were then cultured with or without R2-7 (100 ng/ml) for 10 or 30 minutes, and fixed with 4% PFA. Nuclei were stained with DAPI. Localization of APP3m and APP3c was visualized using a confocal laser microscope. (C) HEK293T-TNFR2 cells were cultured with or without R2-7 (100 ng/ml) for 10 or 30 minutes. Recovered cells were separated into cytosolic and mitochondrial fractions by differential centrifugation. APP3m and APP3c detected by western blotting in each fraction were quantified by densitometric measurement of bands. Images from three independent experiments are shown. Results are mean±s.d., n = 3. **P<0.01 (Student's t-test). (D) APP3 enzymatic activity (mean±s.d.) in the cytosolic (squares) and mitochondrial fractions (triangles) was measured using a fluorescence assay after stimulation with or without R2-7 (100 ng/ml). *P<0.05, **P<0.01 (Student's t-test) compared with the unstimulated control group.
To quantify the changes in the amount of APP3m and APP3c, the intensity of each APP3 band was determined by densitometric measurement. Expression of APP3m increased in the cytoplasmic fraction and decreased markedly in the mitochondrial fraction after TNFR2 stimulation, whereas APP3c intensity in the cytoplasm was almost unchanged (Fig. 5C). In addition, the enzymatic activity of APP3 tended to increase in the cytoplasmic fraction, but decrease in the mitochondrial fraction after TNFR2 stimulation (Fig. 5D). A similar alteration of overall APP3 levels in the mitochondria and cytoplasm was observed in densitometric measurement and enzymatic activity analysis. These results indicate that APP3m translocates from mitochondria to cytoplasm after a TNFR2 activation signal, because overall APP3 expression remained approximately constant in the cell lysate.
Mitochondrial APP3 regulates JNK phosphorylation
To further characterize APP3 functions, we next examined whether APP3m influenced TNFR2 intracellular signaling. TNFR2 is known to induce transcription factors such as NF-κB and AP-1 (Till et al., 2005; Cabal-Hierro and Lazo, 2012). Therefore, we analyzed the activation of MAPKs [p38 MAPK (MAPK14), ERK1/2 (MAPK3 and MAPK1, respectively) and JNK1/2 (MAPK8 and MAPK9, respectively)] as well as NF-κB and phosphoinositide 3-kinase (PI3K) and Akt signals, which are known to occur downstream of TNFR2 signaling (Rao et al., 1995; Jupp et al., 2001; Nicholson and Anderson, 2002). These signals also characterize the TNFR1 pathway and crosstalk through TRAF2, which is a known adaptor molecule for both TNFR1 and TNFR2. TNFR2-specific signal transduction was followed by using R2-7 to eliminate the influence of the TNFR1 signal. Western blot analysis showed that phosphorylation of JNK1/2 and p38 MAPK increased upon TNFR2 stimulation in HEK293T-TNFR2 cells, whereas ERK1/2 was poorly phosphorylated (Fig. 6A; supplementary material Fig. S3A). Notably, in HEK293T-TNFR2 cells that transiently overexpressed APP3m, JNK1/2 phosphorylation reached its maximum level 10 minutes after TNFR2 stimulation (Fig. 6A), but phosphorylation of p38 MAPK and ERK1/2 was not affected (supplementary material Fig. S3A). By contrast, phosphorylation of JNK1/2 and p38 MAPK in APP3c overexpressing cells was unaffected as compared with untransfected cells. Furthermore, phosphorylation of JNK1/2 was decreased by APP3 gene silencing using short hairpin RNA (shRNA) (Fig. 6A). Treatment of HEK293T-TNFR2 with 100 µM apstatin also suppressed phosphorylation of p38 MAPK and ERK1/2, as well as JNK1/2 (supplementary material Fig. S3A). This result indicates the possibility that apstatin inhibited APP1 or APP2 as well as APP3, because apstatin can broadly inhibit aminopeptidase P family proteins (supplementary material Fig. S4). By contrast, stimulation of TNFR2 by R2-7 did not phosphorylate inhibitor of NF-κB (IκB) as previously reported (Rauert et al., 2010). IκB was also not phosphorylated upon overexpression of APP3m or APP3c (Fig. 6B). It is known that Akt is activated by TNFR2 stimulation (Fischer et al., 2011a). R2-7 stimulation also induced phosphorylation of Akt (supplementary material Fig. S3B). However, no alteration in phosphorylated Akt associated with regulation of APP3m or APP3c was observed.
Phosphorylation of JNK and IκB is induced by APP3 during TNFR1 or TNFR2 signaling. (A) HEK293T-TNFR2 cells transfected with APP3m or APP3c, or APP3 shRNA, were prepared. To inhibit aminopeptidase P enzymatic activity, HEK293T-TNFR2 cells were pre-treated with 100 µM apstatin. Untransfected cells were used as a reference. These cells were stimulated with R2-7 (100 ng/ml) for the indicated time. After cell lysis, western blotting was performed to confirm expression of APP3 and TNFR2, as well as phosphorylation of JNK (P-JNK) JNK1 and JNK2 are indicated by the open arrow and filled arrow, respectively. β-actin served as a loading control. (B) IκB and phospho-IκB were also detected in each HEK293T-TNFR2 cell line by western blotting. (C) HEK293T cells transfected with APP3m or APP3c, or APP3 shRNA, and pre-treated with 100 µM apstatin were stimulated by TNF (100 ng/ml) for the indicated time. After cell lysis, JNK and phospho-JNK (JNK1, open arrow; JNK2, filled arrow) were detected by western blotting. (D) IκB and phospho-IκB were also detected in each HEK293T cell line.
Phosphorylation of JNK and IκB is induced by APP3 during TNFR1 or TNFR2 signaling. (A) HEK293T-TNFR2 cells transfected with APP3m or APP3c, or APP3 shRNA, were prepared. To inhibit aminopeptidase P enzymatic activity, HEK293T-TNFR2 cells were pre-treated with 100 µM apstatin. Untransfected cells were used as a reference. These cells were stimulated with R2-7 (100 ng/ml) for the indicated time. After cell lysis, western blotting was performed to confirm expression of APP3 and TNFR2, as well as phosphorylation of JNK (P-JNK) JNK1 and JNK2 are indicated by the open arrow and filled arrow, respectively. β-actin served as a loading control. (B) IκB and phospho-IκB were also detected in each HEK293T-TNFR2 cell line by western blotting. (C) HEK293T cells transfected with APP3m or APP3c, or APP3 shRNA, and pre-treated with 100 µM apstatin were stimulated by TNF (100 ng/ml) for the indicated time. After cell lysis, JNK and phospho-JNK (JNK1, open arrow; JNK2, filled arrow) were detected by western blotting. (D) IκB and phospho-IκB were also detected in each HEK293T cell line.
We considered that APP3m-mediated JNK activation might be induced through TNFR2 in HEK293T-TNFR2 cells. To assess whether activation of the signals occurred through TNFR1, parental HEK293T cells, which mainly express TNFR1, were also incubated with wtTNF. A small amount of phosphorylated JNK1/2 (phospho-JNK1/2) was observed in the untransfected cell line, and this amount increased in APP3m-transfected cells, APP3c-transfected cells and APP3-knockdown cells (Fig. 6C). Furthermore, phosphorylation of IκB increased immediately after TNF stimulation in each type of HEK293T cells (Fig. 6D), and IκB gradually decreased, as previously reported (Wicovsky et al., 2007). Therefore, expression of APP3 protein caused no effects on TNFR1 signaling. Taken together, these results reveal that JNK activation by APP3m is a TNFR2-specific signal because APP3m did not influence the signal through TNFR1.
To assess whether APP3 enzymatic activity is necessary for JNK activation through TNFR2, we tried to create novel APP3m mutants lacking peptidase activity (APP3m dead mutants). Based on the X-ray crystallographic structure of Escherichia coli APP3 (EcAPPro) (Graham et al., 2004), homologous regions of the human APP3 sequence were predicted (Erşahin et al., 2005). In human APP3, it was predicted that His313 would be required for holding substrate; in addition, Asp341 or Glu474 would be the Mn2+-binding site required for enzymatic catalysis (Fig. 7A). Therefore, vectors expressing H313A, D341A and E474A mutants of APP3m were constructed and transfected into HEK293T-TNFR2 cells. APP3m mutants purified by anti-HA immunoprecipitation from these cells were detected at the expected molecular mass (Fig. 7B), and did show loss of enzymatic activity (Fig. 7C). Interestingly, phosphorylation of JNK1/2 was observed in cells overexpressing these mutants, as well as in cells overexpressing APP3m, whereas the level of phosphorylation was low in both cells overexpressing APP3c and untransfected cells (Fig. 7D). In addition, these mutants still retained the ability to bind TNFR2 upon R2-7 stimulation (Fig. 7E). These findings suggest that the enzymatic activity of APP3m is not essential for APP3m-mediated JNK activation,
JNK activation and TNFR2-binding ability of APP3m mutant without enzymatic activity. (A) APP3m dead mutants (H313A, D341A or E474A) were constructed as point mutations as shown schematically. (B) The HA-tagged APP3m, APP3c and APP3m mutant proteins were expressed in HEK293T-TNFR2 cells. After cell lysis, western blotting was performed to confirm protein expression. (C) The HA-tagged APP3m, APP3c and APP3m mutant proteins, which were expressed in HEK293T-TNFR2 cells, were purified by anti-HA immunoprecipitation. Enzymatic activity of purified proteins was measured with an APP fluorogenic substrate peptide. Results are mean±s.d., n = 3. (D) Cells transfected with the APP3m mutants were stimulated with or without R2-7 (100 ng/ml) for 10 minutes. After cell lysis, JNK and phospho-JNK in the cell lysate were detected by western blotting. JNK1 and JNK2 are indicated by the open arrow and filled arrow, respectively. The total intensity of phospho-JNK1/2 (shown by the numbers below the image) was quantified by densitometric measurement of bands from three independent experiments, and a representative image is shown. (E) HA-tagged APP3m mutants were overexpressed in HEK293T-TNFR2. Cells were stimulated with R2-7 (100 ng/ml) for 30 minutes, followed by anti-HA immunoprecipitation (IP). Immunoprecipitates were examined for APP3 and TNFR2 by western blotting to estimate the TNFR2-binding ability of APP3m mutants.
JNK activation and TNFR2-binding ability of APP3m mutant without enzymatic activity. (A) APP3m dead mutants (H313A, D341A or E474A) were constructed as point mutations as shown schematically. (B) The HA-tagged APP3m, APP3c and APP3m mutant proteins were expressed in HEK293T-TNFR2 cells. After cell lysis, western blotting was performed to confirm protein expression. (C) The HA-tagged APP3m, APP3c and APP3m mutant proteins, which were expressed in HEK293T-TNFR2 cells, were purified by anti-HA immunoprecipitation. Enzymatic activity of purified proteins was measured with an APP fluorogenic substrate peptide. Results are mean±s.d., n = 3. (D) Cells transfected with the APP3m mutants were stimulated with or without R2-7 (100 ng/ml) for 10 minutes. After cell lysis, JNK and phospho-JNK in the cell lysate were detected by western blotting. JNK1 and JNK2 are indicated by the open arrow and filled arrow, respectively. The total intensity of phospho-JNK1/2 (shown by the numbers below the image) was quantified by densitometric measurement of bands from three independent experiments, and a representative image is shown. (E) HA-tagged APP3m mutants were overexpressed in HEK293T-TNFR2. Cells were stimulated with R2-7 (100 ng/ml) for 30 minutes, followed by anti-HA immunoprecipitation (IP). Immunoprecipitates were examined for APP3 and TNFR2 by western blotting to estimate the TNFR2-binding ability of APP3m mutants.
Mitochondrial APP3 affects TNF-induced cell death
It is known that TNF induces caspase-dependent programmed cell death (apoptosis), but the role of APP3m in TNF-induced cell death is unclear. To determine the functional effects of APP3m expression in cell death, a cytotoxic assay was performed. After 24 hours of TNF stimulation, the viability of HEK293T-TNFR2 cells was decreased as compared with parental HEK293T cells (Fig. 8A). Previous reports have shown that TNFR2 has a ligand-passing function (Tartaglia et al., 1993; Weiss et al., 1997; Jupp et al., 2001). We examined whether APP3 affected TNF-induced cell death using HEK293T-TNFR2 cells. Two APP3 shRNAs (corresponding to different target sequences, termed APP3 shRNA A and B), and scrambled shRNA were transfected into HEK293T-TNFR2 cells, and a substantial decrease in APP3 expression was confirmed in the shRNA A and B cells (Fig. 8B). Subsequently, these cells were treated with TNF for 24 and 48 hours. We found that the cell lines transfected with APP3 shRNA showed increased cell death after treatment with TNF for 24 hours, whereas those transfected with scrambled shRNA showed no difference in cell death in comparison with mock-transfected cells (Fig. 8C). Cell death was enhanced in both cell lines transfected with APP3 shRNA for 48 hours. However, in HEK293T-TNFR2 cells pre-treated with apstatin, cell death was not induced by TNF after 48 hours in comparison with untreated cells (Fig. 8D). These results indicate that partial inhibition of the TNFR2 signal caused by suppressing APP3 expression promotes TNF-induced cell death, but that the extent of cell death is not affected by inhibition of APP3 enzymatic activity.
Induction of TNF-induced cell death by APP3 knockdown. (A) HEK293T and HEK293T-TNFR2 cells cultured in a 96-well plate were treated with serially diluted TNF. After 24 hours, cell viability was measured by a WST-8 assay. Results are mean±s.d., n = 3. (B) HEK293T-TNFR2 cells were transfected with APP3 shRNA A, APP3 shRNA B or scrambled shRNA, and incubated for 48 hours. After cell lysis, suppression of APP3 was confirmed by western blotting. β-actin served as a loading control. (C) HEK293T-TNFR2 cells were transfected with APP3 shRNA A, APP3 shRNA B or scrambled shRNA. After 48 hours, these cells were treated with TNF (100 ng/ml) for 24 or 48 hours. Mock transfected cells were used as a reference. Cell viability was measured by a WST-8 assay. (D) HEK293T-TNFR2 cells pretreated with 100 µM apstatin were treated with TNF (100 ng/ml) for 24 or 48 hours. Cell viability was measured by WST-8 assay. Results are mean±s.d., n = 3.
Induction of TNF-induced cell death by APP3 knockdown. (A) HEK293T and HEK293T-TNFR2 cells cultured in a 96-well plate were treated with serially diluted TNF. After 24 hours, cell viability was measured by a WST-8 assay. Results are mean±s.d., n = 3. (B) HEK293T-TNFR2 cells were transfected with APP3 shRNA A, APP3 shRNA B or scrambled shRNA, and incubated for 48 hours. After cell lysis, suppression of APP3 was confirmed by western blotting. β-actin served as a loading control. (C) HEK293T-TNFR2 cells were transfected with APP3 shRNA A, APP3 shRNA B or scrambled shRNA. After 48 hours, these cells were treated with TNF (100 ng/ml) for 24 or 48 hours. Mock transfected cells were used as a reference. Cell viability was measured by a WST-8 assay. (D) HEK293T-TNFR2 cells pretreated with 100 µM apstatin were treated with TNF (100 ng/ml) for 24 or 48 hours. Cell viability was measured by WST-8 assay. Results are mean±s.d., n = 3.
DISCUSSION
Although TNF receptors, especially TNFR1, have been well analyzed, the role and signaling of TNFR2 is highly debated. In this study, we attempted to discover new adaptor molecules of TNFR2 to further elucidate TNFR2 signaling mechanisms. To focus on the analysis of TNFR2, we utilized the TNF mutant R2-7, which can bind to TNFR2 selectively, because wtTNF binds to TNFR1 preferentially (Grell et al., 1995; Abe et al., 2011). Because R2-7 has a high specificity for TNFR2, this property offered a distinct advantage in our efforts to discover adaptor molecules of TNFR2. Most proteins involved in signal transduction participate in signaling complexes in which they interact with other proteins, rather than functioning alone. Therefore, we attempted to pull down previously unrecognized adaptor molecules as parts of ligand–receptor complexes (Fig. 1). Because the results of affinity purification of these complexes depend on TNFR2 signaling, the complexes were not isolated from parental HEK293T cells, where expression levels of TNFR2 are barely detectable. Instead, a novel cell line that stably expressed TNFR2 (HEK293T-TNFR2) was established and used to purify the TNFR2 signaling complex. After purifying the TNFR2 signaling complex, APP3 was identified as a potential novel adaptor molecule in the TNFR2 signaling complex using a proteomics approach (Fig. 2A).
Aminopeptidase P family proteins belong to the M24B subfamily of metallopeptidases; there are three different isozymes, APP1 (also known as XPNPEP1), APP2 (also known as XPNPEP2) and APP3 (Erşahin et al., 2005). APP1 and APP2, which are proline-specific exopeptidases, specifically remove the N-terminal amino acid from proteins with a proline residue located in the second position. Gene expression analysis using human cDNA has previously measured the expression levels of both APP3m and APP3c in human tissues (Erşahin et al., 2005). These isoforms were identified in various tissues. The highest levels were in heart followed by pancreas, kidney, testis and peripheral blood mononuclear cells (PBMCs) and other tissues. Notably, a genome-wide homozygosity mapping study of families presenting with the autosomal recessive kidney disease nephronophthisis (NPHP) detected homozygous frameshift and splice-site mutations in the gene encoding APP3 (Böttinger, 2010; O'Toole et al., 2010). This earlier study revealed that APP3, which is related to ciliary dysfunction, is a potential disease-causing protein in kidney. However, there is little information about the substrates and molecular functions of APP3. Possible non-genetic factors, for example, the potential role of TNF in enhancing cyst development in autosomal recessive polycystic kidney disease (ARPKD), which is a disease similar to nephronophthisis (NPHP), have also been suspected. TNF proteins are markedly increased after renal injury and urinary tract infection, which are commonly encountered in this disease (Li et al., 2008). For example, increased levels of TNF-encoding mRNA were found in the kidney of the cpk mouse, a model of ARPKD (Nakamura et al., 1993). An inhibitor of TNF-converting enzyme (TACE) has also been shown to ameliorate polycystic disease in the bpk mouse, which is another model of ARPKD (Dell et al., 2001). These symptoms might be related to TNFR1 function; however, TNFR2 signaling might also be important because of the crosstalk between TNFR1 and TNFR2. It is unclear whether APP3 mediates TNFR2 signal transduction, and adaptor molecules of TNFR2 with proteolytic activities similar to that of APP3 have not been reported. Accordingly, we expected to discover adaptor molecules with molecular functions similar to those of APP3 in the TNFR2 signaling complex.
The present study has demonstrated the behavior of APP3 in TNFR2 signaling. Characterization of the binding ability of APP3 and TNFR2 revealed that only APP3m, which is located in mitochondria, bound specifically to TNFR2. It was presumed that APP3m participated in TNFR2 signaling as an adaptor molecule. APP3m and APP3c have exactly the same amino acid sequences except for a 79-residue domain at the N-terminus of APP3m. Therefore, this N-terminal region might include the site that interacts with TNFR2 and be responsible for the different binding behaviors of these APP3s. Indeed, it was confirmed that N-terminal residues 54–79 of APP3m were important for interaction with TNFR2, because an APP3m mutant in which residues 1–53 were absent, retained binding ability (Fig. 3F).
It is well known that mitochondria-dependent apoptosis is a result of TNFR1 signaling (Schütze et al., 2008). TNFR1 activation evokes mitochondrial outer membrane permeabilization (MOMP), and pro-apoptotic proteins such as cytochrome c, HTRA2 and DIABLO located in the mitochondrial intermembrane space are released to the cytosol. These proteins activate the caspase cascade indirectly and induce apoptosis. In the same manner, recruitment of APP3m is necessary to induce TNFR2 activation. Thus, APP3m would need to relocate from mitochondria to the cytoplasm to interact with TNFR2 in the plasma membrane, because APP3m is mostly located in mitochondria. However, the mitochondrial proteins involved in TNFR2 signaling have not yet been fully characterized. MOMP was not observed in the early phase of either TNFR1 or TNFR2 signaling (Fig. 4A,B). Furthermore, the kinetics of intracellular APP3m suggested that translocation of APP3m from mitochondria to the cytoplasm depends on activation of a TNFR2 signal (Fig. 5). It is possible that the translocation of APP3m occurs independently of MOMP.
We found that APP3m was capable of inducing phosphorylation of JNK in TNFR2 signaling (Fig. 6A). However, it was unclear whether the enzymatic activity of APP3m was required for JNK activation. We constructed three novel point mutations of APP3m because there have been no reports of human APP3m mutants. We found that JNK activation induced by APP3m did not involve its enzymatic activity, because the APP3m dead mutants still activated JNK (Fig. 7). Our findings demonstrate a new mechanism by which APP3m regulates JNK phosphorylation in TNFR2 signal transduction, although further analysis is needed to fully characterize the signaling pathway leading to phosphorylation of JNK and to clarify the contribution to other JNK-activating receptors. These findings might support the hypothesis that APP3 is involved in AP-1 activation through the MEKK1, MKK4, MKK7 to JNK signaling pathway (Qi and Elion, 2005).
At present, the physiological significance of APP3m localization in mitochondria is unknown. Perhaps APP3m is released to the cytoplasm only at the time of signal transduction to prevent harmful effects on other proteins, because APP3m is an adaptor molecule with protease activity. We found that suppression of APP3 expression increased TNF-dependent cell death (Fig. 8). Because inhibition of APP3 by use of apstatin did not significantly affect cell death, however, the amount of APP3 that binds to TNFR2 might be important. It is possible that the APP3m-mediated TNFR2 signal has the potential to play an anti-apoptotic role.
Anti-TNF drugs have been shown to have beneficial effects in the treatment of several autoimmune diseases, including rheumatoid arthritis, multiple sclerosis and psoriasis. However, these drugs sometimes lead to adverse effects because they prevent signaling though both TNFR1 and TNFR2 (Lamprecht, 2005; Van Hauwermeiren et al., 2011). It has recently been reported that TNFR2 signaling might play a protective role in autoimmune diseases, and TNFR2 has received much attention as a therapeutic target. In several cases, its effect has been clearly defined and successfully tested (Faustman and Davis, 2010; Liu, 2011). For example, it seems that activation of TNFR2 signaling is a selective means of destroying pathogenic autoreactive CD8+ T cells in blood taken from patients with type 1 diabetes (Ban et al., 2008). This suggests that specific control of APP3 function might modulate TNFR2 signaling by a means other than through a TNFR2-specific agonist or antibody. Additional studies to further characterize TNFR2 signaling will be important to elucidate the molecular pathogenesis and to develop improved therapeutic drugs.
MATERIALS AND METHODS
Cell culture, antibodies, and reagents
HEK293T cells were maintained in Dulbecco's modified Eagle's medium (DMEM) (Wako Pure Chemical, Osaka, Japan) supplemented with 10% fetal bovine serum and 1% antibiotic mixture (10,000 units/ml penicillin, 10 mg/ml streptomycin and 25 µg/ml amphotericin B) (Wako Pure Chemical). The biotinylated antibodies for human TNFR1 or human TNFR2 and phycoerythrin-labeled streptavidin, for cell surface staining, were purchased from BD (Franklin Lakes, NJ). For western blotting, the biotinylated antibodies against human TNFR1 and TNFR2 were purchased from R&D Systems (Minneapolis, MN). Horseradish peroxidase (HRP) streptavidin conjugate was purchased from ZYMED Laboratories (South San Francisco, CA). The antibody against human TRAF2 was purchased from Santa Cruz Biotechnology (Santa Cruz, CA). The antibodies for human APP3, cytochrome c, HTRA2, DIABLO were purchased from Abcam (Cambridge, UK). The anti-human antibodies against p38, phospho-p38, ERK1/2, phospho-ERK1/2, JNK, phospho-JNK, IκB, phospho-IκB, Akt, phospho-Akt, COX IV, VDAC and the secondary antibody conjugated to HRP were purchased from Cell Signaling Technology (Danvers, MA). The antibody against β-actin (AC-74) was from Sigma Aldrich (St Louis, MO). Apstatin was purchased from Santa Cruz Biotechnology. MitoTracker Red CMXRos was purchased from Invitrogen (Carlsbad, CA). The APP fluorogenic substrate, H-Lys(Abz)-Pro-Pro-pNA, was purchased from Bachem (Bubendorf, Switzerland).
Plasmid construction
The human TNFR2 gene was amplified by PCR from human peripheral blood lymphocyte cDNA. The resulting amplified fragment was cloned into the entry vector pENTR1A (Invitrogen). The recombination reaction, called the LR reaction, was then performed to transfer the TNFR2 gene into pcDNA6.2/V5-DEST (Invitrogen), and an expression vector encoding human TNFR2 (pcDNA6.2-TNFR2) was constructed. The human APP3m (XPNPEP3 isoform 1, UniProt entry, Q9NQH7-1) and human APP3c (XPNPEP3 isoform 2, Uniprot entry, Q9NQH7-2) genes were amplified by PCR from a human XPNPEP3 cDNA (Promega, Madison, WI) with two different forward primers. To construct a vector encoding a C-terminal HA-tagged APP3, each of the resultant PCR products were then cloned into a pMEX-HA mammalian expression vector (Dualsystems Biotech AG, Zurich, Switzerland) at an SfiI site (to create pMEX-APP3m-HA and pMEX-APP3c-HA, respectively). Expression vectors for the APP3m MTS mutant, APP3m MTS deletion mutants and APP3m dead mutants were constructed based on pMEX-APP3m-HA. In brief, for deletion of the MTS domain, inverse PCR was performed using primer sets designed to amplify outwards from amino acid 1–45 or 1–53. For point mutation, inverse PCR was performed with primer sets designed to replace Arg18, Arg29, Arg30, Arg39, Arg40 and Arg44 residues with alanine residues (pMEX-APP3m MTSΔR-HA), or to replace His313, Asp341 or Glu474 with alanine residues (pMEX-APP3m(H313A)-HA, pMEX-APP3m(D341A)-HA and pMEX-APP3m(E474A)-HA, respectively). To create C-terminal Venus (a yellow fluorescent protein) fusion APP3 constructs, each APP3 gene obtained by PCR was also cloned into a pTriEx-3-Venus vector (Millipore) (pTriEx-3-APP3m-Venus and pTriEx-3-APP3c-Venus, respectively).
Generation of cells stably expressing TNFR2
pcDNA6.2-TNFR2 was transfected to HEK293T cells by lipofection methods using Lipofectamine LTX (Invitrogen) according to the manufacturer's recommended protocol. After 24 hours, cells were cultured with medium containing 8 µg/ml blasticidin S (Invitrogen). After about 3 weeks, TNFR2-positive cells were sorted using a cell sorter (FACSAria, BD). Resultant cells that stably expressed TNFR2 were maintained in DMEM supplemented with 10% fetal bovine serum (FBS), 1% antibiotic mixture and 5 µg/ml blasticidin S.
Flow cytometry
HEK293T or HEK293T-TNFR2 cells (5×105 cells each) were suspended in PBS containing 2% FBS. Cells were incubated with biotinylated antibodies specific for human TNFR1 (0.5 µg/ml) or human TNFR2 (0.5 µg/ml) for 30 min. The cells were then washed three times and incubated for 30 min with PE-labeled streptavidin. Expression levels of each receptor were measured using a flow cytometer (FACSCanto, BD). 10,000 cells were analyzed per sample. Cells incubated without antibody or with an isotype control antibody were measured as references simultaneously. Data were evaluated using FlowJo (Tree Star, Ashland, OR).
Affinity purification of the TNF–TNFR2 signaling complex
HEK293T-TNFR2 cells (∼1×108 cells), were treated with R2-7–FLAG (100 ng/ml) or wtTNF–FLAG (100 ng/ml) for 30 min at 37°C. After washing twice with PBS, the recovered cells were lysed in 1 ml of lysis buffer [50 mM Tris-HCl pH 7.4, 150 mM NaCl, 1 mM EDTA, 1% Triton X-100, 50 mM NaF, 30 mM Na4P2O7·10H2O, 1 mM Na3VO4, and protease inhibitor cocktail (Roche Applied Science, Upper Bavaria, Germany)] and gently rocked at 4°C for 15 min. The samples were then centrifuged at 20,000 g for 30 minutes and the supernatants were incubated with Sepharose CL-4B beads (Sigma Aldrich) for 1 hour. The resulting lysates were incubated with an anti-FLAG M2 agarose affinity gel (Sigma Aldrich) for 1 hour at 4°C. The recovered gels were washed with wash buffer (500 mM Tris-HCl pH 7.4, 1.5 M NaCl). The immunoprecipitates were eluted competitively from the gel by incubation with a 3×FLAG peptide (Sigma Aldrich) at a concentration of 150 µg/ml. The 3×FLAG peptide included in the solution was eliminated by ultrafiltration using an Amicon YM-10 membrane (Millipore, Billerica, MA).
Mass spectrometry and protein identification
The TNFR2 signaling complex purified by immunoprecipitation was reduced with 5 mM tris(2-carboxyethyl)phosphine hydrochloride (TCEP-HCl, Sigma Aldrich) and alkylated with 10 mM iodoacetamide (Sigma Aldrich), followed by trypsin (100 µg/ml) digestion for 16 hours at 37°C. The digested peptides were purified using OMIX Pipette Tips C18 (Varian, Palo Alto, CA) and dissolved in 0.1% (v/v) formic acid. This sample was then sequenced using an LTQ-Orbitrap hybrid mass spectrometer (Thermo Fisher Scientific, Waltham, MA) equipped with a reversed-phase liquid chromatography system. Proteins identified by mass spectrometry were assigned a molecular weight search (MOWSE) score, which was expressed as a protein score using a Mascot search engine (http://www.matrixscience.com) querying the entire theoretical peptide mass in the NCBI and SwissProt database (http://www.expasy.org/, a public domain database provided by the Swiss Institute of Bioinformatics). The search query was configured as follows: (1) the peptides were mono-, di- or tri-isotopic, (2) methionine residues could be oxidized, (3) all cysteine residues were modified with carbamidomethyl.
Immunoprecipitation and immunoblotting
For FLAG-tag purification, HEK293T-TNFR2 cells were seeded in a 100-mm dish and incubated with R2-7–FLAG (100 ng/ml). They were then lysed in a lysis buffer at 4°C. The R2-7–TNFR2 complex was purified with an anti-FLAG M2 agarose affinity gel as described above. For HA-tag purification, pMEX-APP3m-HA and pMEX-APP3c-HA, respectively, were transfected into HEK293T-TNFR2 cells by lipofection. After 24 hours, these cells, which transiently expressed APP3, were stimulated by TNF (100 ng/ml) or R2-7 (100 ng/ml). After cell lysis, the supernatant obtained by centrifugation (20,000 g for 30 minutes) was incubated with an EZview Red anti-HA affinity gel (Sigma Aldrich) at 4°C for 1 hour. The recovered gel was washed in lysis buffer and the bound proteins were eluted by competition with 150 µg/ml of an HA peptide (Sigma Aldrich).
The cell lysates or resultant immunoprecipitation eluates were separated by SDS-PAGE and transferred onto PVDF membranes (Immobilon-P, Millipore). After blocking with 4% Block Ace (DS Pharma Biomedical, Osaka, Japan) to prevent nonspecific binding, the membranes were probed with the indicated antibodies and visualized using enhanced chemiluminescence with ECL prime (GE Healthcare, Buckinghamshire, UK) for the detection of proteins. Equivalence of loading proteins was confirmed by use of the β-actin signal.
Measurement of APP3 enzymatic activity
Each sample was added to a 96-well black plate (Thermo Fisher Scientific). Next, 100 µM H-Lys(Abz)-Pro-Pro-pNA was added to each well. After incubation for 15 min at 37°C, fluorescence intensity was measured using a fluorescence plate reader (EnSpire, PerkinElmer, Waltham, MA). The excitation and emission wavelengths were 320 nm and 410 nm, respectively.
Fluorescence microscopy
HEK293T and HEK293T-TNFR2 cells (1×105 cells/well each) were seeded in a two-well chamber glass slide. After incubation for 24 hours, cells were treated with TNF (100 ng/ml) or R2-7 (100 ng/ml) for 30 minutes. Cells were also treated with FCCP (20 µM), a depolarization agent, for 10 min as a positive control. Then, TMRE staining was performed using a TMRE mitochondrial membrane potential assay kit (Abcam) according to the manufacturer's recommended protocol. In brief, TMRE was added to cells in medium at a final concentration of 100 nM and incubated for 20 minutes at 37°C. After washing with PBS, TMRE staining of mitochondria in live cells was observed using a fluorescence microscope (IX81, Olympus, Tokyo, Japan)
HEK293T-TNFR2 cells (3×104 cells/well) were seeded in a collagen-type-I-coated two-well chamber slide (Asahi Techno Glass, Shizuoka, Japan) and cultured overnight. For transient expression of APP3m or APP3c fused to Venus (a yellow fluorescent protein), pTriEx-3-APP3m-Venus (200 ng) and pTriEx-3-APP3c-Venus (200 ng) were respectively transfected by lipofection. After 24 hours, cells were incubated with 200 nM MitoTracker Red CMXRos (Invitrogen) for 30 minutes to stain the mitochondria, and they were then stimulated with R2-7 (100 ng/ml) for 10 and 30 minutes, respectively. Stimulated cells were fixed with PBS containing 4% paraformaldehyde (PFA) for 30 minutes on ice. Cells were subsequently mounted using Vectashield Mounting Medium with DAPI (Vector Laboratories, Burlingame, CA) to stain the nuclei. The APP3 localization was determined by scanning with a confocal laser scanning microscope (Leica TCS SP2, Leica, Wetzlar, Germany).
TMRE fluorescence microplate assay
HEK293T or HEK293T-TNFR2 cells (3×103 cells/well each) were seeded in a 96-well clear-bottomed plate (Thermo Fisher Scientific). As described above, after 24 hours of incubation, cells were treated with TNF (100 ng/ml), R2-7 (100 ng/ml) or FCCP (20 µM). The cells were then incubated with 500 nM TMRE for 20 min at 37°C. After washing, TMRE-stained cells were observed using a fluorescence plate reader. The excitation and emission wavelengths were 549 nm and 575 nm, respectively.
Subcellular fractionation and semi-quantification of APP3
After collection of HEK293T or HEK293T-TNFR2 cells (∼1×107 cells each), separation of cytosolic and mitochondrial fractions was performed by using a mitochondria isolation kit for cultured cells (Thermo Fisher Scientific) according to the manufacturer's recommended protocol.
For quantification of APP3, HEK293T-TNFR2 cells seeded on a 100-mm dish were treated with R2-7 (100 ng/ml). After collection of cells (∼2×106 cells), cell lysates or cellular fractions were prepared as described above. The APP3m or APP3c was contained in each sample was detected by western blotting. Optical densities of the APP3 bands were calculated using Image J. Integrated optical densities were corrected for background intensities, which were based on the values obtained for untreated samples.
Knockdown and inhibition of APP3
For APP3 transient knockdown, a human APP3 shRNA plasmid (OriGene Technologies, Rockville, MD) was transfected into HEK293T-TNFR2 cells using Lipofectamine LTX. After culture for 48 hours, the cells were used for APP3 inhibition assays. For inhibition of APP3 enzymatic activity, HEK293T-TNFR2 cells were pre-treated with 100 µM apstatin (Santa Cruz Biotechnology) for 30 minutes at 37°C.
APP3m dead mutations
pMEX-APP3m(H313A)-HA, pMEX-APP3m(D341A)-HA or pMEX-APP3m(E474A)-HA was transfected into HEK293T-TNFR2 cells by lipofection. After 24 hours of incubation, cell lysates were prepared. Anti-HA immunoprecipitation was perfomed on each cell lysate, and the enzymatic activity of each resultant immunoprecipitation eluate was measured. In addition, cells expressing the APP3m dead mutants were treated with R2-7 (100 ng/ml) for 10 min. After, preparation of cell lysates and immunoprecipitation eluates, the JNK activation and TNF-binding ability of each mutant was assessed by western blotting.
Cell death assay
HEK293T-TNFR2 cells (1×105 cells/well) were seeded in a 96-well plate. Two APP3 shRNA plasmids, each with a different target sequence (APP3 shRNA A, 5′-AGACCAGACAGTGGTTGTGCTCTCCAACC-3′; and B, 5′-GATGGAGGTTGTGAGTCTTCCTGCTATGT-3′), and a scrambled negative control shRNA plasmid (OriGene) were transfected into the cells by lipofection. After 48 hours of incubation, the cells were treated with TNF (100 ng/ml), along with cells pre-treated with 100 µM apstatin. After 24 or 48 hours, the viability of cells was evaluated by a colorimetric assay using Cell Count Reagent SF (WST-8, Nakarai Tesque, Kyoto, Japan).
Author contributions
M.I. and H.K. designed the study, performed experiments and wrote the manuscript. Y.A. designed the study and performed the proteomic experiment. K.H., K.N., Y.M., Y.Y. and Y.T. gave valuable advice on the research. S.T. directed the research and assisted in writing and editing the manuscript. All authors provided comments on the manuscript.
Funding
This study was supported in part by Grants-in-Aid for Scientific Research [grant numbers 24680093 to H.K., 24390022 to S.T.] from the Ministry of Education, Culture, Sports, Science and Technology of Japan. This study was also supported in part by Health Labour Sciences Research Grants from the Ministry of Health, Labor and Welfare of Japan.
References
Competing interests
The authors declare no competing or financial interests.




![Recruitment of APP3m but not APP3c to TNF–TNFR2 complex. (A) APP3 has two differentially localized isoforms. APP3m (57 kDa) has an N-terminal mitochondrial-targeting sequence (MTS) domain, and is imported into mitochondria where it localizes as a 51-kDa mature enzyme. APP3c (48 kDa), lacking MTS, is expressed in the cytosol. An NCBI search for conserved domains predicted an aminopeptidase P, N-terminal domain (AMP_N) and prolidase domain in each APP3. (B) In HEK293T-TNFR2 cells, transiently expressing APP3m and APP3c were detected as 51-kDa and 48-kDa proteins, respectively, as described in A. APP3m in which arginine residues are replaced with alanine residues in the MTS domain (APP3m MTSΔR), was expressed as a protein of ∼57 kDa, although its expression level was low. APP3m was mostly present as the 51-kDa protein in APP3m-transfected cells. (C) HEK293T-TNFR2 cells that transiently expressed APP3m–HA or APP3c–HA were stimulated with TNF (100 ng/ml) or R2-7 (100 ng/ml) for 30 minutes. Anti-HA immunoprecipitation (IP) showed that R2-7, as well as TNF, recruited APP3m to TNFR2, but APP3c was not recruited. (D) Anti-FLAG immunoprecipitation was performed using APP3-transfected HEK293T-TNFR2 after R2-7–FLAG (100 ng/ml) stimulation. Western blotting confirmed that endogenous APP3m was detected in cells transfected with both APP3m–HA and APP3c–HA. However, transfected APP3 was detected only in the APP3m–HA transfectant with anti-HA antibody. (E) Aminopeptidase P activity was measured in anti-FLAG immunoprecipitates. Only elutes from cells transfected with APP3m–HA, and not APP3c–HA, showed higher enzymatic activity. Results are mean±s.d., n = 3. **P<0.01 (Student's t-test). (F) APP3m–HA mutants, in which the MTS domain 1–45 [APP3m MTSΔ(1–45)–HA] or 1–53 [APP3m MTSΔ(1–53)–HA] was deleted, were expressed in cells. After R2-7 (100 ng/ml) stimulation for 30 min, anti-HA immunoprecipitation was performed. Western blotting showed that these mutants bound to TNFR2 as indicated in the schematic in the right-hand panel, and that a 26-amino-acid sequence (shaded region in the schematic) was essential for TNFR2 binding. (G) HEK293T-TNFR2 cells were treated with R2-7–FLAG (100 ng/ml) for the indicated time. After cell lysis, to confirm time-dependent recruitment of APP3 to the receptor, anti-FLAG immunoprecipitation was performed followed by western blotting. (H) HA-tagged APP3m (APP3m–HA) or APP3c-HA was transiently expressed in HEK293T-TNFR2 cells. R2-7 (100 ng/ml) stimulation followed by anti-HA immunoprecipitation was performed to determine the time-dependent manner of APP3m or APP3c recruitment to the TNFR2 signaling complex. Western analysis was performed with anti-APP3, anti-TNFR2 or anti-TRAF2 antibody.](https://cob.silverchair-cdn.com/cob/content_public/journal/jcs/128/4/10.1242_jcs.149385/4/m_jcs-128-04-0656-f03.jpeg?Expires=1716300194&Signature=Pbp81eC9PsMMy4E7poCg0AMzZ-vuvvctRxpIFDnbZWK1PfenNrOtbE2GgqIjQxUbg9T59HluORSV1N29a1Eq2PyoVP7BgKbIKW1PmfUwgkOTOrvq2if0YgtGom~vhRcKv-FpSUy4Fk5O8jRomlEUrmZbW6jufgkITQwlQor57QWoWjS2MfuaHOC8BEgbkbsPElhSqZVRWpcY3LNv3-FgnL7nOWdFHrpm83uz2Zvf8TTik-8si6zupk9abggtk7SNib-0zAfUYH8HAk6bc-yNca-BZ8yPifzzMaDzXGGv6lGVP-xPor-BBd7v1CNYVVNmO9u8vNGpu3~uT5f1t5pSEA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)