Summary
Chemokines have recently been reported to be involved in pathological bone destruction. However, the physiological roles of chemokines in bone metabolism in vivo have not been well documented. We analyzed the bone phenotypes in Cx3cr1-deficient mice. The mice exhibited slight but significant increases in trabecular and cortical thickness, reduced numbers of osteoclasts and increased rates of osteoid formation. Although the morphometric parameters showed marginal differences, the Cx3cr1-deficient bones showed an elevated expression of Osterix/SP7, which encodes an essential transcriptional factor for osteoblasts, whereas the gene Osteocalcin/Bglap, which encodes a late marker, was downregulated. The levels of transcripts for various osteoclastic markers, such as receptor activator of NF-κB (RANK)/TNFRSF11A, receptor activator of NF-κB ligand (RANKL)/TNFSF11, tartrate-resistant acid phosphatase 5b (TRAP5B)/ACP5B, Cathepsin K(CTSK), MMP3 and MMP13, were significantly decreased in the Cx3cr1-deficient bones. Cultured Cx3cr1-deficient osteoblastic cells showed inverse temporal patterns of osteoblastic marker expression and reduced calcium deposition. Furthermore, in vitro studies and immunofluorescence staining against CX3CR1 and CX3CL1 suggested a role for the CX3CR1–CX3CL1 axis in an early stage of osteoblast differentiation, possibly through their trans and cis interactions. Cultured Cx3cr1-deficient pre-osteoclasts showed impaired differentiation, mainly due to a deficiency of the CD115+CD11blo osteoclastogenic population of myeloid-lineage precursors. The treatment of bone-marrow-derived osteoclastic cultures with recombinant CX3CL1 at different time points suggested that the CX3CR1–CX3CL1 axis favors the maintenance of osteoclastic precursors, but not differentiated osteoclasts. These observations uncovered novel roles of the CX3CR1–CX3CL1 axis in the differentiation of both osteoblasts and osteoclasts.
Introduction
Chemokines were originally identified as a group of structurally-related cytokines that direct the homing of circulating leukocytes to sites of inflammation (Charo and Ransohoff, 2006). These ligands bind to cell surface molecules that comprise a group of seven transmembrane Gαi protein-coupled receptors. Chemokines are categorized into four subfamilies according to the arrangement of conserved cysteine residues located in their N-terminal ends: CXC, CC, C and CX3C. In addition to these systematically categorized chemokine families, another related family of chemokine-like factors (CKLF) has been characterized (Han et al., 2001; Han et al., 2003; Wang et al., 2006). CKLF1 is a cytokine with a total of 99 residues, and is a functional ligand for CCR4. It has a CC motif that is identical to that of CCL17 and CCL22, but lacks the additional C-terminus cysteines possessed by other CC chemokines. A group of proteins unrelated structurally to chemokines but having chemokine-like functions, such as HMGB1, macrophage migration inhibitory factor (MIF) and interleukin (IL)-6, is proposed to be named CLF (chemokine-like functions) (Degryse and de Virgilio, 2003; Noels et al., 2009).
Several recent studies have reported that some chemokines are responsible for pathological bone destruction through their regulation of osteoclasts and their precursor cells, which are derived from common progenitor cells in the bone marrow. Some reports have suggested that CCL2 (also called MCP-1) is highly expressed by osteoblasts in response to parathyroid hormone (Li et al., 2007), while its specific receptor, CCR2, has been reported to be involved in postmenopausal bone loss in ovariectomy-induced bone loss models (Binder et al., 2009). In addition, CCL3 (also called MIP-1α), a major proinflammatory chemokine produced at sites of inflammation, stimulates osteoclastogenesis (Kim et al., 2006; Menu et al., 2006; Oba et al., 2005) and bone resorption in multiple myeloma (Choi et al., 2000; Han et al., 2001; Haringman et al., 2006; Yang et al., 2006), thus indicating it to be a crucial chemokine involved in pathological bone destruction. Another chemokine, CX3CL1 (also called fractalkine), a unique membrane-bound form of chemokine like CXCL16 (Ludwig and Mentlein, 2008; Sheikine and Sirsjö, 2008; Shimaoka et al., 2004; Shimaoka et al., 2007) that exerts dual functions as a chemoattractant and adhesion molecule (Imai et al., 1997), was also reported to be involved in osteoclastogenesis (Koizumi et al., 2009; Saitoh et al., 2007). Although these results suggest that CX3CR1 regulates the differentiation and function of osteoclasts, the roles of CX3CR1 in bone homeostasis are still not fully understood. Such knowledge is crucial for optimizing the treatments targeting chemokines to prevent pathogenic bone resorption. Therefore, it is important to investigate the bone phenotypes in chemokine receptor-deficient mice in order to better understand the physiological roles of chemokines.
We recently demonstrated that Ccr1-deficient (Ccr1−/−) mice develop osteopenia due to the impaired function of osteoblasts and osteoclasts, which led us to discuss the possibility of using CCR1-related chemokine ligands as therapeutic targets. Bone cells derived from Ccr1−/− mice show diminished expression levels of several chemokine ligands, thus suggesting that hierarchal networks of chemokines participate in bone metabolism (Hoshino et al., 2010). Therefore, in the present study, we investigated the bone features of Cx3cr1-deficient mice to further assess the roles of the chemokine receptors in bone metabolism. Both in vivo and in vitro observations demonstrated the critical roles of the CX3CR1–CX3CL1 axis in maintaining bone homeostasis by regulating the functional differentiation of osteoblasts and osteoclasts, as well as bone cell communication.
Results
The bone phenotypes in Cx3cr1-deficient mice suggest possible roles in bone formation, as well as bone resorption
To understand the functions of CX3CR1 in bone metabolism, we first investigated the bone structure of Cx3cr1-deficient mice using microCT. The microCT images indicated the presence of slightly increased cancellous trabeculae in the Cx3cr1-deficient mice compared to that observed in wild-type mice (Fig. 1A). Quantitative analyses showed slightly elevated parameters of the bone volume per tissue volume (BV/TV), trabecular thickness (Tb.Th.), cortical thickness (Ct.Th.) and trabecular volume (Tb.V.) compared to those observed in wild-type mice, although the trabecular separation (Tb.Sp.) and trabecular number (Tb.N.) did not show significant difference (Fig. 1B). Bone histomorphometric analyses showed higher values of bone volume per tissue volume (BV/TV), osteoid volume (OV/BV), osteoid surface (OS/BS) and bone formation rates (BFR/BS) in the Cx3cr1-deficient mice compared to wild-type mice, although the osteoid thickness (O.Th.), osteoblast surface per bone surface (Ob.S/BS), mineral apposition rate (MAR) and the mineralized surface (MS/BS) showed no significant differences between the mice (Fig. 1C). More importantly, the bone histomorphometric analysis showed significant decreases in parameters associated with bone resorption, such as osteoclast numbers (N.Oc./B.Pm) and osteoclast surface areas (Oc.S/BS) (Fig. 1D), which appears to be consistent with a previous report in which anti-CX3CL1 Abs-injected mice exhibited lower scores for the bone resorption index compared to the control IgG-injected mice (Koizumi et al., 2009). Although these parameters of pQCT and from the bone histomorphometric analyses showed marginal differences between wild-type and Cx3cr1-deficient mice, they suggested possible roles for Cx3cr1 in bone formation, as well as in bone resorption.
Immature osteoblasts and reduced numbers of osteoclasts in Cx3cr1-deficient mice. (A) microCT images of the femurs in wild-type and Cx3cr1-deficient mice. (B) The bone analyses of distal femurs of wild-type (open bars) and Cx3cr1-deficient (filled bars) mice using the microCT analysis in A. Parameters relating to the trabecular structure: bone volume per tissue volume (BV/TV), trabecular thickness (Tb.Th.), cortical bone thickness (Ct.Th.), trabecular separation (Tb.Sp.), trabecular volume (Tb.V.) and trabecular number (Tb.N.). *Significant increases compared to wild-type littermate controls, P<0.05. (C,D) The bone histomorphometric analyses of the distal femurs of wild-type (open bars) and Cx3cr1-deficient (filled bars) mice. Parameters relating to trabecular structure and bone formation in C: bone volume per tissue volume (BV/TV), osteoid volume to bone volume (OV/BV), osteoid surface/bone surface (OS/BS), osteoid thickness (O.Th.), osteoblast surface per bone surface (Ob.S/BS), mineral apposition rate (MAR), mineralizing surface per bone surface (MS/BS) and formation rate referenced to the bone surface (BFR/BS). Parameters relating to bone resorption in D: osteoclast number per bone perimeter (N.Oc./B.Pm) and osteoclast surface per bone surface (Oc.S/BS). The bone histomorphometric analysis data are represented as the means ± s.e.m. obtained from eight mice in each group. * and # indicate a significant upregulation and downregulation, respectively (P<0.05) from wild-type controls, P<0.05.
Immature osteoblasts and reduced numbers of osteoclasts in Cx3cr1-deficient mice. (A) microCT images of the femurs in wild-type and Cx3cr1-deficient mice. (B) The bone analyses of distal femurs of wild-type (open bars) and Cx3cr1-deficient (filled bars) mice using the microCT analysis in A. Parameters relating to the trabecular structure: bone volume per tissue volume (BV/TV), trabecular thickness (Tb.Th.), cortical bone thickness (Ct.Th.), trabecular separation (Tb.Sp.), trabecular volume (Tb.V.) and trabecular number (Tb.N.). *Significant increases compared to wild-type littermate controls, P<0.05. (C,D) The bone histomorphometric analyses of the distal femurs of wild-type (open bars) and Cx3cr1-deficient (filled bars) mice. Parameters relating to trabecular structure and bone formation in C: bone volume per tissue volume (BV/TV), osteoid volume to bone volume (OV/BV), osteoid surface/bone surface (OS/BS), osteoid thickness (O.Th.), osteoblast surface per bone surface (Ob.S/BS), mineral apposition rate (MAR), mineralizing surface per bone surface (MS/BS) and formation rate referenced to the bone surface (BFR/BS). Parameters relating to bone resorption in D: osteoclast number per bone perimeter (N.Oc./B.Pm) and osteoclast surface per bone surface (Oc.S/BS). The bone histomorphometric analysis data are represented as the means ± s.e.m. obtained from eight mice in each group. * and # indicate a significant upregulation and downregulation, respectively (P<0.05) from wild-type controls, P<0.05.
Impaired expression of osteoblastic and osteoclastic markers in Cx3cr1-deficient mice
To investigate the status of osteoblasts and osteoclasts in the bones of Cx3cr1-deficient mice, we compared the transcript levels of osteoblast- and osteoclast-related markers in the femurs of wild-type and Cx3cr1-deficient mice. Fig. 2A summarizes the changes in the expression levels of transcripts of osteoblast-related markers including transcription factors (Runx2 and Osterix/SP7) (Ducy et al., 1997; Komori et al., 1997; Liu et al., 2001) and bone matrix proteins [Collagen1a1 (Col1a1), Osteonectin (SPARC) and Osteocalcin (BGLAP)]. Osterix was significantly upregulated (by ∼170%) in the Cx3cr1-deficient femurs compared to that observed in the femurs of the wild-type mice, whereas the Runx2 level was not significantly different. Among the genes encoding bone matrix proteins, Osteonectin was significantly upregulated, and Osteocalcin, which encodes a marker of mature osteoblasts, was significantly downregulated, in the Cx3cr1-deficient mice (Fig. 2A). The expression level of Collagen1a1 did not show any significant differences between the Cx3cr1-deficient and wild-type mice (Fig. 2A). These results suggest that Cx3cr1 regulates both the differentiation and function of osteoblasts.
The expression of genes related to osteoblasts and osteoclasts in Cx3cr1-deficient mice. (A) Transcripts of osteoblast-related transcription factors (Runx2 and Osterix) and osteoblastic markers (Collagen1a1, Osteonectin and Osteocalcin) extracted from the bone tissue of wild-type (open bars) and Cx3cr1-deficient mice (filled bars) were measured using a real-time quantitative PCR (RT-PCR) analysis (mean ± s.e.m., n = 8). n.d., not detected. (B) The expression levels of transcripts of osteolytic markers, bone-resorption enzymes (Trap5b, CathepsinK) and bone-related MMPs (Mmp3 and Mmp13) were analyzed using mRNA extracted from bone tissue from wild-type (open bars) and Cx3cr1-deficient mice (filled bars). (C) The serum levels of TRAP5b (wild-type, n = 10; Cx3cr1-deficient, n = 8), NTX (wild-type and Cx3cr1-deficient, n = 8) and BALP (wild-type, n = 10; Cx3cr1-deficient, n = 8) in wild-type (open bars) and Cx3cr1-deficient male mice (filled bars) aged 9–13 weeks were measured using ELISAs. Horizontal lines indicate the means. (D,E) The expression levels of (D) Rank, Rankl and Osteoprotegerin and (E) specific chemokine of CX3CR1, Cx3cr1, chemokine receptor Ccr1 and chemokines Ccl5 and Ccl9, extracted from the bone tissue of wild-type (open bars) and Cx3cr1-deficient (filled bars) mice were measured using a RT-PCR analysis (means ± s.e.m., n = 8). n.d., not detected.
The expression of genes related to osteoblasts and osteoclasts in Cx3cr1-deficient mice. (A) Transcripts of osteoblast-related transcription factors (Runx2 and Osterix) and osteoblastic markers (Collagen1a1, Osteonectin and Osteocalcin) extracted from the bone tissue of wild-type (open bars) and Cx3cr1-deficient mice (filled bars) were measured using a real-time quantitative PCR (RT-PCR) analysis (mean ± s.e.m., n = 8). n.d., not detected. (B) The expression levels of transcripts of osteolytic markers, bone-resorption enzymes (Trap5b, CathepsinK) and bone-related MMPs (Mmp3 and Mmp13) were analyzed using mRNA extracted from bone tissue from wild-type (open bars) and Cx3cr1-deficient mice (filled bars). (C) The serum levels of TRAP5b (wild-type, n = 10; Cx3cr1-deficient, n = 8), NTX (wild-type and Cx3cr1-deficient, n = 8) and BALP (wild-type, n = 10; Cx3cr1-deficient, n = 8) in wild-type (open bars) and Cx3cr1-deficient male mice (filled bars) aged 9–13 weeks were measured using ELISAs. Horizontal lines indicate the means. (D,E) The expression levels of (D) Rank, Rankl and Osteoprotegerin and (E) specific chemokine of CX3CR1, Cx3cr1, chemokine receptor Ccr1 and chemokines Ccl5 and Ccl9, extracted from the bone tissue of wild-type (open bars) and Cx3cr1-deficient (filled bars) mice were measured using a RT-PCR analysis (means ± s.e.m., n = 8). n.d., not detected.
The expression levels of genes of osteoclasts-related markers, such as Trap5b/Acp5b and Cathepsin K (Ctsk), were significantly attenuated in the Cx3cr1-deficient mice compared to those observed in the wild-type mice (Fig. 2B). The expression levels of Mmp3 and Mmp13, encoding bone-specific matrix metalloproteinases, were also decreased in the Cx3cr1-deficient mice (Fig. 2B). Furthermore, the Cx3cr1-deficient mice showed significantly decreased serum levels of TRAP5b (Delmas, 1993) and collagen-type I N-telopeptides (NTx) (Schneider and Barrett-Connor, 1997; Takahashi et al., 1997) (Fig. 2C).
Since these results supported the presence of diminished osteoclastic bone resorption in the Cx3cr1-deficient mice, we assessed the activation of the RANK–RANKL axis, an essential signaling pathway in the osteoblast–osteoclast interactions that regulates osteoclast differentiation and function. Interestingly, both Rank/Tnfrsf11a and Rankl/Tnfsf11 were significantly downregulated in the Cx3cr1-deficient mice compared to the levels observed in wild-type mice (Fig. 2D). Notably, a soluble osteoclastogenesis inhibitory factor gene, Osteoprotegerin (OPG)/Tnfrsf11b, was significantly upregulated in the Cx3cr1-deficient mice (Fig. 2D), implying that a lack of CX3CR1 impairs osteoclastogenesis through the RANK–RANKL axis.
We further investigated the expression levels of transcripts for CX3CL1, a specific and unique ligand of CX3CR1, CCR1, another chemokine receptor, and its bone-specific ligands, CCL5 and CCL9, in the bones of Cx3cr1-deficient mice (Fig. 2E), since we had previously reported critical roles of the CCR1 axis involving CCL5 and CCL9 in the differentiation and function of both osteoblasts and osteoclasts by observing Ccr1-deficient mice (Hoshino et al., 2010). Interestingly, the expression of Cx3cl1, Ccr1 and Ccl9 was almost completely eliminated, and the level of Ccl5 was significantly downregulated in the bones from Cx3cr1-deficient mice (Fig. 2E).
Attenuated differentiation and function in osteoblastic cells isolated from Cx3cr1-deficient mice
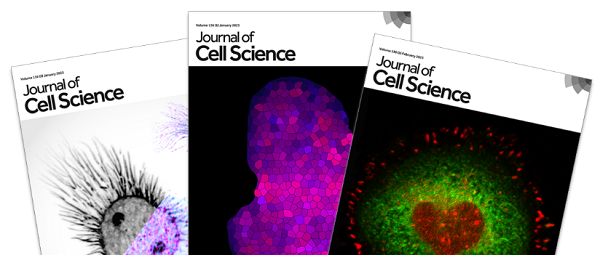
To elucidate the roles of CX3CR1 in osteoblast differentiation and function, we cultured osteoblastic cells derived from Cx3cr1-deficient mice and compared their phenotypes with those from wild-type mice. We first noted that there was significantly reduced calcium deposition (Fig. 3A) in the Cx3cr1-deficient osteoblastic cells compared to that observed in the cells of wild-type mice. We next assessed the transcriptional levels of osteoblastic markers using a real-time quantitative PCR (RT-PCR) analysis (Fig. 3B). The temporal expression levels of Runx2 and Osterix in the Cx3cr1-deficient cells were inverted compared to those observed in the wild-type cells. On day 14, the Runx2 expression level was lower, and the Osterix expression level was higher, in the Cx3cr1-deficient osteoblastic cells than in the cells from the wild-type mice. The Cx3cr1-deficient cells showed significantly lower transcription levels of bone-specific alkaline phosphatase (Balp)/Alpl, Collagen1a1 and Osteonectin on days 0 and 14, and higher levels on day 21, than those observed in the wild-type cells. The Osteocalcin level in the wild-type osteoblasts was dramatically upregulated on day 21; however, its transcription level in the Cx3cr1-deficient osteoblastic cells was suppressed throughout the culture period. The temporal expression patterns of the osteoblastic markers suggest that there is a maturation disorder in the Cx3cr1-deficient osteoblastic cells.
Impairment of osteoblast differentiation in CX3CR1-deficient cells. (A) Osteoblastic cells isolated from wild-type (open bars) and Cx3cr1-deficient mice (filled bars) were cultured. The mineralized nodules were stained using von Kossa's method and the samples were photographed. The number of mineralized nodules was calculated (means ± s.e.m., n = 4), and the calcium content in the nodules was measured and normalized to the DNA content in the lysates (means ± s.e.m., n = 4; right graph). (B) The relative expression levels of transcripts of osteoblastic transcription factors (Runx2 and Osterix) and markers (Balp, Collagen1a1, Osteonectin and Osteocalcin) by immature (day 14, before mineral deposition) or mature (day 21, with mineralization) osteoblastic cells isolated from wild-type (open circle) and Cx3cr1-deficient mice (filled circle) were measured using RT-PCR (means ± s.e.m. n = 8). The statistical significance was determined with the Tukey–Kramer HSD test. * and # indicate a significant upregulation and downregulation, respectively (P<0.05) compared with unstimulated stromal cells (P<0.05). There were significant differences between wild-type and Cx3cr1-deficient cells, with significant upregulation denoted by ⋆ and downregulation by ★, respectively (P<0.05). (C,D) Co-culture of osteoblasts and osteoclasts from wild-type and Cx3cr1-deficient mice. (C) The relative expression levels of Rankl and Osteoprotegerin by the osteoblastic cells derived from wild-type (open circles) and Cx3cr1-deficient mice (filled circles) were measured using RT-PCR (means ± s.e.m., n = 8). (D) Osteoclasts were induced from wild-type osteoclast precursors by co-culture with osteoblasts of wild-type and Cx3cr1-deficient mice. (Left panels) Multinuclear osteoclasts were visualized with TRAP chromogenic stain on osteoblastic cells derived from wild-type and Cx3cr1-deficient mice (magnification ×100). (Right panel) The number of TRAP+ multinuclear osteoclasts was counted (means ± s.e.m., from duplicate experiments, n = 3). Osteoclast culture with M-CSF and RANKL without osteoblasts were carried out as positive controls. #Significant differences from the co-culture of osteoclasts with wild-type osteoblasts, P<0.05. (E) The relative expression levels of Cx3cr1, Cx3cl1 and Ccr1 by the immature and mature osteoblastic cells from wild-type (open circles) and Cx3cr1-deficient mice (filled circles) as measured by RT-PCR (means ± s.e.m., n = 6). The difference between the wild-type and Cx3cr1-deficient cells was statistically significant [downregulation (★), N.D. not detected]. (F) Chemokines (CCL5 and CCL9) in the culture supernatants of wild-type and Cx3cr1-deficient osteoblastic cells were measured using ELISAs (means ± s.e.m., duplicated, n = 4).
Impairment of osteoblast differentiation in CX3CR1-deficient cells. (A) Osteoblastic cells isolated from wild-type (open bars) and Cx3cr1-deficient mice (filled bars) were cultured. The mineralized nodules were stained using von Kossa's method and the samples were photographed. The number of mineralized nodules was calculated (means ± s.e.m., n = 4), and the calcium content in the nodules was measured and normalized to the DNA content in the lysates (means ± s.e.m., n = 4; right graph). (B) The relative expression levels of transcripts of osteoblastic transcription factors (Runx2 and Osterix) and markers (Balp, Collagen1a1, Osteonectin and Osteocalcin) by immature (day 14, before mineral deposition) or mature (day 21, with mineralization) osteoblastic cells isolated from wild-type (open circle) and Cx3cr1-deficient mice (filled circle) were measured using RT-PCR (means ± s.e.m. n = 8). The statistical significance was determined with the Tukey–Kramer HSD test. * and # indicate a significant upregulation and downregulation, respectively (P<0.05) compared with unstimulated stromal cells (P<0.05). There were significant differences between wild-type and Cx3cr1-deficient cells, with significant upregulation denoted by ⋆ and downregulation by ★, respectively (P<0.05). (C,D) Co-culture of osteoblasts and osteoclasts from wild-type and Cx3cr1-deficient mice. (C) The relative expression levels of Rankl and Osteoprotegerin by the osteoblastic cells derived from wild-type (open circles) and Cx3cr1-deficient mice (filled circles) were measured using RT-PCR (means ± s.e.m., n = 8). (D) Osteoclasts were induced from wild-type osteoclast precursors by co-culture with osteoblasts of wild-type and Cx3cr1-deficient mice. (Left panels) Multinuclear osteoclasts were visualized with TRAP chromogenic stain on osteoblastic cells derived from wild-type and Cx3cr1-deficient mice (magnification ×100). (Right panel) The number of TRAP+ multinuclear osteoclasts was counted (means ± s.e.m., from duplicate experiments, n = 3). Osteoclast culture with M-CSF and RANKL without osteoblasts were carried out as positive controls. #Significant differences from the co-culture of osteoclasts with wild-type osteoblasts, P<0.05. (E) The relative expression levels of Cx3cr1, Cx3cl1 and Ccr1 by the immature and mature osteoblastic cells from wild-type (open circles) and Cx3cr1-deficient mice (filled circles) as measured by RT-PCR (means ± s.e.m., n = 6). The difference between the wild-type and Cx3cr1-deficient cells was statistically significant [downregulation (★), N.D. not detected]. (F) Chemokines (CCL5 and CCL9) in the culture supernatants of wild-type and Cx3cr1-deficient osteoblastic cells were measured using ELISAs (means ± s.e.m., duplicated, n = 4).
We next investigated the osteoclast-supporting activities in cultured osteoblastic cells. Cx3cr1-deficient osteoblastic cells expressed significantly lower and higher levels of Rankl and Osteoprotegerin, respectively, throughout the culture period compared to those observed in wild-type osteoblastic cells (Fig. 3C). This result is consistent with our in vivo observations of bone tissue from Cx3cr1-deficient mice (as shown in Fig. 2D). We next performed co-cultures of wild-type pre-osteoclasts with osteoblastic cells isolated from either wild-type or Cx3cr1-deficient mice. As expected, a significantly reduced number of osteoclasts was formed from the co-cultures with Cx3cr1-deficient osteoblastic cells compared to those with wild-type osteoblastic cells (Fig. 3D). Treatment with pertussis toxin (PTX), an inhibitor of Gαi-protein-coupled receptors that is involved in chemokine signaling, prevented the wild-type osteoblastic cells from generating substantial numbers of osteoclasts (Fig. 3C), confirming the requirement of Gαi protein-mediated signal for osteoclastgenesis as previously reported (Hoshino et al., 2010).
We then investigated the transcript expression levels of CX3CR1, its unique ligand, CX3CL1, and another chemokine receptor, CCR1, in osteoblastic cell cultures (Fig. 3E). The temporal expression patterns showed that the level of Cx3cr1 transcription on days 0 and 14 was significantly higher than that on day 21, suggesting that there was downregulation of the Cx3cr1 transcript depending on the maturation of osteoblasts. The level of Cx3cl1 was greatly upregulated on day 14 only in the wild-type osteoblastic cells. In contrast, the level of Cx3cl1 in Cx3cr1-deficient osteoblastic cells was dramatically suppressed, and was maintained at the basal level throughout the culture period. These temporal patterns of Cx3cr1 and Cx3cl1 expression suggest that the interaction between the receptor and the ligand likely occurs at an early stage of osteoblast differentiation, but not a late stage of mineralization.
The transcriptional level of Ccr1 was significantly downregulated throughout the culture period in Cx3cr1-deficient mice compared to that observed in wild-type mice. The secretion of CCL5 and CCL9, critical ligands for CCR1 required for osteoblast differentiation (Hoshino et al., 2010), were also significantly reduced in Cx3cr1-deficient osteoblastic cells (Fig. 3F). These findings suggest that osteoblastic phenotypes in Cx3cr1-deficient mice involve the reduced function of the CCR1 axis.
Predominant expression of CX3CR1 and CX3CL1 proteins in osteoblasts in trabecular bone compared to those in lining cells on the cortical bone surface
The in vivo expression of the CX3CR1 and CX3CL1 proteins in osteoblasts was investigated by immunofluorescence using antibodies specific for the proteins in tissue sections of tibiae from 4-week-old mice. Specific signals against CX3CR1 and CX3CL1 were predominantly detected in the cuboidal osteoblasts covering primary trabeculae adjacent to the growth plate cartilage (Fig. 4A, upper panels). In the mid-shaft region, faint signals for these proteins were observed in the cells lining the endosteum on the cortical bone surface (Fig. 4A, lower panels, indicated by arrowheads), while intense signals were detected in bone marrow cells.
The expression of CX3CR1 and CX3CL1 proteins in osteoblasts in vivo and in vitro. (A) Immunofluorescence studies using specific antibodies against CX3CR1 and CX3CL1 were carried out on sections of tibiae from 4-week-old mice. CX3CR1 and CX3CL1 were detected by secondary antibodies conjugated with Alexa Fluor 568 (in red). Sections were counterstained with DAPI to detect nuclei (in blue). Differential interference contrast (DIC) images of each section were obtained for morphological observation. Scale bars: 20 µm. The dotted lines demarcate the border between the growth plate (GP) cartilage and primary trabeculae (TB). The arrows indicate endosteum lining cells. BM, bone marrow; CB, cortical bone. (B) Double immunostaining for CX3CR1 and CX3CL1 was carried out on MC3T3-E1 cells. CX3CR1 and CX3CL1 were detected by secondary antibodies conjugated with Alexa Fluor 568 (in red) and 488 (in green), respectively. Sections were counterstained with DAPI to detect nuclei (in blue). Merged images are shown in the right panels. Scale bars: 50 µm.
The expression of CX3CR1 and CX3CL1 proteins in osteoblasts in vivo and in vitro. (A) Immunofluorescence studies using specific antibodies against CX3CR1 and CX3CL1 were carried out on sections of tibiae from 4-week-old mice. CX3CR1 and CX3CL1 were detected by secondary antibodies conjugated with Alexa Fluor 568 (in red). Sections were counterstained with DAPI to detect nuclei (in blue). Differential interference contrast (DIC) images of each section were obtained for morphological observation. Scale bars: 20 µm. The dotted lines demarcate the border between the growth plate (GP) cartilage and primary trabeculae (TB). The arrows indicate endosteum lining cells. BM, bone marrow; CB, cortical bone. (B) Double immunostaining for CX3CR1 and CX3CL1 was carried out on MC3T3-E1 cells. CX3CR1 and CX3CL1 were detected by secondary antibodies conjugated with Alexa Fluor 568 (in red) and 488 (in green), respectively. Sections were counterstained with DAPI to detect nuclei (in blue). Merged images are shown in the right panels. Scale bars: 50 µm.
We next carried out the same immunofluorescence studies on MC3T3-El osteoblastic cells to investigate their subcellular localizations in these cells. Double labeling of the CX3CR1 and CX3CL1 proteins demonstrated that both proteins were mostly colocalized in the cytoplasm and surface of the cells in the pre-confluent state (Fig. 4B, upper panels). Interestingly, they were also detected in the cellular processes that connected cells to each other. However, in sub-confluent state, only a few cells showed intense signals for CX3CR1 and CX3CL1, while most of the cells exhibited very faint signals (Fig. 4B, lower panels). These observations were consistent with the temporal expression patterns of Cx3cr1 and Cx3cl1 in osteoblastic cell cultures derived from bones (Fig. 3E), thus suggesting that their interaction occurs during an early stage of osteoblast differentiation.
Recombinant CX3CL1 stimulates the expression of osteoblastic transcriptional factors
To further investigate the roles of the CX3CL1–CX3CR1 axis, we inoculated the soluble form of recombinant mouse CX3CL1 (rmCX3CL1) into the primary osteoblastic cell cultures from wild-type bones and observed its effects on the expression of bone markers by RT-PCR (Fig. 5). The rmCX3CL1 strongly stimulated the expression of Runx2 and Osterix in a dose-dependent manner. The Collagen1a1 level was significantly stimulated by 50 ng/ml rmCX3CL1, but was downregulated by a higher dose (100 ng/ml). Only the highest dose of rmCX3CL1 (100 ng/ml) significantly inhibited the expression of Balp, Osteopontin/Spp1 and Osteocalcin. The endogenous Cx3cl1 expression was dose-dependently downregulated, while the Rankl level was not significantly affected by rmCX3CL1. Therefore, CX3CL1 stimulates the expression of transcription factors that are essential for osteoblastogenesis and the early function of osteoblasts.
Enhancement of Runx2 and Osterix expression by treatment with recombinant CX3CL1 in a dose-dependent manner. The relative expression levels of osteoblastic markers and Cx3cl1 in wild-type osteoblasts treated with rmCX3CL1 (10, 50 and 100 ng/ml) were determined by RT-PCR. The data were compared with the wild-type osteoblasts stimulated with control vehicle (means ± s.e.m., n = 3). The statistical significance was determined by the Tukey–Kramer HSD test. * and # indicate a significant upregulation and downregulation, respectively (P<0.05) between control and rmCX3CL1 stimulation.
Enhancement of Runx2 and Osterix expression by treatment with recombinant CX3CL1 in a dose-dependent manner. The relative expression levels of osteoblastic markers and Cx3cl1 in wild-type osteoblasts treated with rmCX3CL1 (10, 50 and 100 ng/ml) were determined by RT-PCR. The data were compared with the wild-type osteoblasts stimulated with control vehicle (means ± s.e.m., n = 3). The statistical significance was determined by the Tukey–Kramer HSD test. * and # indicate a significant upregulation and downregulation, respectively (P<0.05) between control and rmCX3CL1 stimulation.
Impaired osteoclast differentiation and bone-resorbing activity in osteoclastic cells isolated from CX3CR1-deficient mice
To further corroborate the necessity of CX3CR1 in osteoclast differentiation and function, we employed in vitro osteoclast culture systems induced from myeloid precursors in the presence of M-CSF and RANKL. We first undertook a morphological examination of osteoclastogenesis in Cx3cr1-deficient osteoclast precursors. The fluorescent staining of F-actin in cultured osteoclasts showed no obvious morphological differences in actin ring formation between the wild-type and Cx3cr1-deficient cells (Fig. 6A, in green). However, there was no detectable staining for Cathepsin K in Cx3cr1-deficient osteoclasts, whereas wild-type cells showed positive signals in mononuclear osteoclast progenitors and multinucleated osteoclastic cells (Fig. 6A, in red). Fig. 6B summarizes the expression levels of osteoclast-related markers as determined by RT-PCR. The expression levels of Rank, Nfat-c1, Trap5b, Cathepsin K, Integrin alphaV (ItgaV) and Integrin beta3 (Itgb3) in Cx3cr1-deficient cells were significantly lower compared to those observed in wild-type cells. In contrast, the expression levels of myeloid-lineage markers, such as S1P1 (Ishii et al., 2009) and Irf-8 (Zhao et al., 2009) in the Cx3cr1-deficient osteoclasts were increased compared to those observed in wild-type cells. In addition, a pit formation assay performed using bone slices demonstrated that wild-type osteoclasts completely resorb both mineralized and unmineralized bone matrices, while Cx3cr1-deficient osteoclasts fail to remove unmineralized bone matrices (Fig. 6C). We therefore conducted a collagen-based zymography study to assess the collagenolytic activity of the osteoclastic cells. This study revealed that the lysates of Cx3cr1-deficient osteoclasts does not fully digest type-I collagens (Fig. 6D).
Impairment of osteoclast functions by CX3CR1 deficiency. (A), Osteoclastic cells were induced from the bone marrow of wild-type and Cx3cr1-deficient mice using M-CSF and RANKL treatment. In vitro osteoclast cultures from wild-type and Cx3cr1-deficient precursors were carried out for 10 days (upper panels) or 17 days (lower panels) and cultures were stained with an anti-CathepsinK polyclonal antibody (red), and for F-actin (green) and nuclei (blue). Scale bar: 50 µm. (B) The relative expression levels of transcripts of osteoclastic differentiation markers on day 4 after culture[RANK and its downstream transcription factor NFATC1; bone-specific enzymes, TRAP5B and CathepsinK protease; osteoclast-specific integrins alphaV and beta3; and myeloid-lineage cell markers S1P1 and IRF-8] in wild-type (open bars) and Cx3cr1-deficient (filled bars) preosteoclasts were measured by RT-PCR (means ± s.e.m., n = 5). *Significantly upregulated, #significantly downregulated compared with wild-type controls, P<0.05. (C) Scanning electron micrographs of the pit formation assay of wild-type and Cx3cr1-deficient osteoclasts. Scale bar: 2 µm. (D) The collagen digestion activity of wild-type and Cx3cr1-deficient osteoclasts was measured using collagen-based zymography. BMM, cell lysates from bone-marrow-derived macrophages (10 µg protein/lane); WT and KO, wild-type and Cx3cr1-deficient osteoclast lysates (1 and 10 µg protein/lane), respectively.
Impairment of osteoclast functions by CX3CR1 deficiency. (A), Osteoclastic cells were induced from the bone marrow of wild-type and Cx3cr1-deficient mice using M-CSF and RANKL treatment. In vitro osteoclast cultures from wild-type and Cx3cr1-deficient precursors were carried out for 10 days (upper panels) or 17 days (lower panels) and cultures were stained with an anti-CathepsinK polyclonal antibody (red), and for F-actin (green) and nuclei (blue). Scale bar: 50 µm. (B) The relative expression levels of transcripts of osteoclastic differentiation markers on day 4 after culture[RANK and its downstream transcription factor NFATC1; bone-specific enzymes, TRAP5B and CathepsinK protease; osteoclast-specific integrins alphaV and beta3; and myeloid-lineage cell markers S1P1 and IRF-8] in wild-type (open bars) and Cx3cr1-deficient (filled bars) preosteoclasts were measured by RT-PCR (means ± s.e.m., n = 5). *Significantly upregulated, #significantly downregulated compared with wild-type controls, P<0.05. (C) Scanning electron micrographs of the pit formation assay of wild-type and Cx3cr1-deficient osteoclasts. Scale bar: 2 µm. (D) The collagen digestion activity of wild-type and Cx3cr1-deficient osteoclasts was measured using collagen-based zymography. BMM, cell lysates from bone-marrow-derived macrophages (10 µg protein/lane); WT and KO, wild-type and Cx3cr1-deficient osteoclast lysates (1 and 10 µg protein/lane), respectively.
Impaired expression of the CCR1 axis in Cx3cr1-deficient osteoclasts
We further investigated whether changes in the CCR1 axis were involved in the Cx3cr1-deficient osteoclast differentiation. First, the time course changes in the expression levels of Cx3cr1 and Ccr1 during the culture period were assessed using wild-type osteoclast precursors (Fig. 7A). The expression level of Cx3cr1 on day 0 was ∼10 times higher than that of Ccr1. The Cx3cr1 expression was rapidly downregulated on day 4, and then was subsequently sustained at a lower level. The transcriptional level of Ccr1 showed a peak on day 4. These results suggest that the expression levels of Cx3cr1 and Ccr1 change depending on the osteoclast maturation stages: a high expression level of Cx3cr1 is observed at an early stage of osteoclastogenesis, while an increased level of Ccr1 is observed during the middle to later stages.
Changes in the CCR1-mediated axis and the osteoclasic precursor population caused by CX3CR1 deficiency. (A) The temporal expression profiles of chemokine receptors Ccr1 and Cx3cr1 by wild-type precursors were measured using RT-PCR (means ± s.d., n = 5). The levels are normalized to the expression of Gapdh. * and # indicate significant upregulation and downregulation, respectively, compared with the levels on day 0 (P<0.05). Osteoclastic cells were induced from the bone marrow of wild-type and Cx3cr1-deficient mice by treatment with M-CSF and RANKL. (B) The expression levels of transcripts of the chemokine receptor CCR1 and bone-related chemokines (CCL9 and CCL5) extracted from osteoclastic cells of wild-type (open bars) and Cx3cr1-deficient mice (filled bars) were measured using a RT-PCR (means ± s.e.m., n = 8). n.d., not detected. (C) Endogenous CCL5 and CCL9 in the culture supernatant of wild-type (open bars) and Cx3cr1-deficient osteoclastic (filled bars) cells were measured using ELISAs (means ± s.e.m., experiments performed in duplicate, n = 3). (D) A population analysis of RANK in CD45+CD11b+CD115+ osteoclastic precursors isolated from the bone marrow of wild-type and Cx3cr1-deficient mice after 4 days in culture was analyzed by flow cytometry. Histograms were gated on the CD11bhiRANK+ (R1-gated) subpopulation and CD11bloRANKdull (R2-gated) subpopulation of CD11b+CD115+ osteoclastic precursors. The surface expression levels of RANK (bold line) are overlaid on cells stained with subclass-matched control IgG (shaded histogram). Plots and histograms are shown as the representative data of three independent experiments, and the population ratio is shown as the mean percentage ± s.e.m. (n = 3).
Changes in the CCR1-mediated axis and the osteoclasic precursor population caused by CX3CR1 deficiency. (A) The temporal expression profiles of chemokine receptors Ccr1 and Cx3cr1 by wild-type precursors were measured using RT-PCR (means ± s.d., n = 5). The levels are normalized to the expression of Gapdh. * and # indicate significant upregulation and downregulation, respectively, compared with the levels on day 0 (P<0.05). Osteoclastic cells were induced from the bone marrow of wild-type and Cx3cr1-deficient mice by treatment with M-CSF and RANKL. (B) The expression levels of transcripts of the chemokine receptor CCR1 and bone-related chemokines (CCL9 and CCL5) extracted from osteoclastic cells of wild-type (open bars) and Cx3cr1-deficient mice (filled bars) were measured using a RT-PCR (means ± s.e.m., n = 8). n.d., not detected. (C) Endogenous CCL5 and CCL9 in the culture supernatant of wild-type (open bars) and Cx3cr1-deficient osteoclastic (filled bars) cells were measured using ELISAs (means ± s.e.m., experiments performed in duplicate, n = 3). (D) A population analysis of RANK in CD45+CD11b+CD115+ osteoclastic precursors isolated from the bone marrow of wild-type and Cx3cr1-deficient mice after 4 days in culture was analyzed by flow cytometry. Histograms were gated on the CD11bhiRANK+ (R1-gated) subpopulation and CD11bloRANKdull (R2-gated) subpopulation of CD11b+CD115+ osteoclastic precursors. The surface expression levels of RANK (bold line) are overlaid on cells stained with subclass-matched control IgG (shaded histogram). Plots and histograms are shown as the representative data of three independent experiments, and the population ratio is shown as the mean percentage ± s.e.m. (n = 3).
We next compared the expression levels of Ccr1, Ccl5 and Ccl9 between Cx3cr1-deficient and wild-type osteoclasts, since they are a critical chemokine receptor and its ligands are required for osteoclast differentiation (Hoshino et al., 2010). The expression levels of Ccr1 and Ccl5 in the Cx3cr1-deficient osteoclasts were significantly downregulated compared to those observed in wild-type mouse-derived osteoclasts, whereas the Ccl9 expression in Cx3cr1-deficient osteoclasts was significantly upregulated (Fig. 7B). These changes in chemokine ligand expression were consistently confirmed at the protein levels in the media from cultured cells (Fig. 7C).
Population changes in osteoclastic precursors associated with CX3CR1 deficiency after RANKL simulation
We examined whether CX3CR1 deficiency affects the population changes in RANK-expressing osteoclast precursors (Fig. 7D). After the culture of bone-marrow-derived cells with M-CSF and RANKL, the cellular profiles of osteoclast precursors were analyzed using a flow cytometric analysis. This analysis revealed that Cx3cr1-deficient mice have slightly higher numbers of CD11b+CD115+ myeloid-lineage precursors compared to wild-type mice (14.35±1.90% in Cx3cr1-deficient mice to 13.40±0.95% in wild-type mice; Fig. 7D; Table 1). However, the subpopulations of osteoclast precursors (R2-gated cells), which express CD11bloRANKdull and are reported to be required for multi-nuclear osteoclasts (Arai et al., 1999; Hoshino et al., 2010), were significantly reduced in Cx3cr1-deficient cells (1.01±0.02% in Cx3cr1-deficient mice to 1.89±0.55% in wild-type mice). In addition, the expression level of RANK in the R2-gated (CD11blo) cells was diminished in Cx3cr1-deficient cells. The population changes in these osteoclastogenic subpopulations likely contribute to the reduced expression of osteoclast markers in Cx3cr1-deficient osteoclastic cells, as observed in Ccr1-deficient osteoclastic cells (Hoshino et al., 2010).
Population analysis of RANK in CD45+CD11b+CD115+ osteoclastic precursors of wild-type, Ccr1-deficient and Cx3cr1-deficient mice
| CD45+ (%) | CD11b+CD115+(%) | CD11bhi (%) | CD11blo (%) | |
| Wild-type | 87.73±4.28 | 13.40±0.95 | 10.99±0.94 | 1.89±0.55 |
| CCR1KO | 91.75±2.33 | 9.67±0.43* | 8.26±0.30* | 0.63±0.09* |
| CX3CR1KO | 91.93±1.53 | 14.35±1.90 | 13.00±1.98 | 1.01±0.02* |
| CD45+ (%) | CD11b+CD115+(%) | CD11bhi (%) | CD11blo (%) | |
| Wild-type | 87.73±4.28 | 13.40±0.95 | 10.99±0.94 | 1.89±0.55 |
| CCR1KO | 91.75±2.33 | 9.67±0.43* | 8.26±0.30* | 0.63±0.09* |
| CX3CR1KO | 91.93±1.53 | 14.35±1.90 | 13.00±1.98 | 1.01±0.02* |
Population ratio of CD11bhi (R1-gated) subpopulation and CD11blo (R2-gated) subpopulation of CD11b+CD115+ osteoclastic precursors (in Fig. 5) is shown as mean percentage ± s.e.m. (n = 3). *Statistically significant (P<0.05), based on post-hoc test of one-factor factorial ANOVA.
Treatment with recombinant CX3CL1 prior to, but not after, RANKL stimulation delays osteoclastic marker expression
To dissociate the temporal roles of the CX3CR1–CX3CL1 axis in osteoclast differentiation in vitro, we treated the bone-marrow-derived osteoclast cultures stimulated by M-CFS and RANKL with rmCX3CL1 at two distinct time points, and analyzed the time-dependent expression levels of osteoclast and myeloid lineage markers by RT-PCR (Fig. 8). Since we noticed that the expression of Cx3cr1 was readily downregulated within 6 hours after RANKL inoculation (Fig. 8A and data not shown), we treated the bone-marrow-derived osteoclast precursors with rmCX3CL1 1 hour prior to RANKL stimulation on day 1. Accordingly, when rmCX3CL1 was inoculated on day 1, the activation of osteoclastic marker genes such as Rank, Nfat-c1, Trap and Cathepsin K was delayed compared to those in cells treated with the control vehicle, whereas the expression of myeloid-lineage marker genes, such as S1P1 and Irf8, was sustained at higher levels than those in the control (Fig. 8A). Consistently, a time-dependent downregulation of the Cx3cr1 level observed in control cells, and was delayed in the treated cells. The expression of Ccr1 in the treated cells was sustained at a low level, while it was upregulated in control. However, the treatment with rmCX3CL1 initiated on day 4 after RANKL stimulation did not lead to any obvious differences between the treated and control cells in terms of their temporal expression patterns of these markers and chemokine receptors (Fig. 8B).
Delay in osteoclastic marker expression after treatment with recombinant CX3CL1 prior to RANKL stimulation. The relative expression levels of transcripts of osteoclastic differentiation markers were measured using a RT-PCR analysis. The levels were normalized to the expression of Gapdh. Cells were cultured with M-CSF and RANKL for 10 days, stimulated with rmCX3CL1 (50 ng/ml) for days 1–10 (triangles), and for days 4–10 (filled circles), then were compared with unstimulated osteoclasts (open circles). *Significantly upregulated mRNA, and #significantly downregulated mRNA compared to the day 1 controls, P<0.05 (means ± s.e.m., n = 3). The differences between unstimulated osteoclasts and rmCX3CL1-treated osteoclasts were significantly increased (⋆P<0.05) and decreased (★P<0.05), respectively.
Delay in osteoclastic marker expression after treatment with recombinant CX3CL1 prior to RANKL stimulation. The relative expression levels of transcripts of osteoclastic differentiation markers were measured using a RT-PCR analysis. The levels were normalized to the expression of Gapdh. Cells were cultured with M-CSF and RANKL for 10 days, stimulated with rmCX3CL1 (50 ng/ml) for days 1–10 (triangles), and for days 4–10 (filled circles), then were compared with unstimulated osteoclasts (open circles). *Significantly upregulated mRNA, and #significantly downregulated mRNA compared to the day 1 controls, P<0.05 (means ± s.e.m., n = 3). The differences between unstimulated osteoclasts and rmCX3CL1-treated osteoclasts were significantly increased (⋆P<0.05) and decreased (★P<0.05), respectively.
Discussion
The roles of the CX3CR1–CX3CL1 axis in osteoblast differentiation
The results of our bone histomorphometric study indicated that there was impaired osteoblast differentiation and function in Cx3cr1-deficient mice (Fig. 1C). Since the roles of the CX3CR1–CX3CL1 axis in osteoblast differentiation have not been fully documented, we further investigated the functional role of the CX3CR1–CX3CL1 axis in osteoblast differentiation. Immunofluorescence staining for CX3CR1 and CX3CL1 on bone specimens revealed that these two proteins were expressed predominantly in the cuboidal cells covering trabecular bone, while faint signals were detected in the flat lining cells on the surface of the cortical bone of the diaphysis. Our previous work demonstrated that the cuboidal cells covering trabecular bone exhibited active beta-catenin signaling and Osterix expression, which are associated with active osteoblast formation and an early stage of osteoblast function (Watanabe et al., 2012). In cultured osteoblastic MC3T3-E1 cells, CX3CR1 and CX3CL1 were detectable in the cytoplasm and cellular processes in their pre-confluent state; however, they appeared to be downregulated in their sub-confluent state and in later stages. These findings, together with the temporal expression patterns of Cx3cr1 and Cx3cl1 observed during cultured osteoblast differentiation (Fig. 3E), suggest that the CX3CR1–CX3CL1 axis plays a role in an early stage of osteoblast differentiation. Furthermore, the subcellular localization of these two proteins suggests possible cis and trans interactions between CX3CL1 and CX3CR1 in osteoblasts.
The cultured osteoblastic cells isolated from Cx3cr1-deficient mice also showed complicated changes in the temporal expression patterns of osteoblastic markers, and decreased calcium deposition (Fig. 3A,B). Runx2 and Osterix encode essential transcription factors for osteoblast commitment and differentiation at an early stage (Kanatani et al., 2006; Komori et al., 1997; Liu et al., 2001; Nakashima et al., 2002). Recently, Yoshida et al. reported that sustained expression of Osterix and Runx2 inhibited osteoblast differentiation from proceeding to a late stage in a reciprocally independent manner (Yoshida et al., 2012). Therefore, it is possible that the inverse temporal downregulation and upregulation of transcription factors such as Runx2 and Osterix, as was observed in vitro (Fig. 3B), may cause spatiotemporally disordered bone matrix deposition that eventually results in impaired mineral deposition, which may contribute to the increased osteoid volume in the bones of Cx3cr1-deficient mice (Fig. 1C). Treatment of wild-type mouse-derived osteoblastic cultures with rmCX3CL1 stimulated the expression of Runx2 and Osterix, but had inhibitory effects on the expression of bone matrix proteins (Fig. 5). Taken together, these findings suggest that the CX3CR1–CX3CL1 axis plays important roles favoring an early stage of osteoblast differentiation, and thus contribute to the regulation of its proper functional maturation.
We also observed a significant suppression of Ccr1 in osteoblastic cells isolated from Cx3cr1-deficient mice throughout the culture period (Fig. 3E). As we previously observed in Ccr1−/− osteoblastic cells, the levels of chemokine ligands for CCR1, such as CCL5 and CCL9, were significantly reduced in Cx3cr1-deficient osteoblastic cells (Fig. 3F). These findings suggest that CX3CR1 acts upstream of CCR1 in a chemokine-dependent amplification loop that sustains or amplifies the chemokine signaling networks involved in osteoblast differentiation, as we previously discussed (Hoshino et al., 2010). Indeed, we observed differences in the temporal expression patterns of Cx3cr1 and Ccr1, wherein Cx3cr1 was upregulated at an early stage and the Ccr1 expression was augmented in a later stage in wild-type osteoblastic cell cultures (Fig. 3E). Therefore, one possible reason for the complex phenotypes of bone formation and osteoblastic dysfunction associated with CX3CR1 deficiency is that the chemokine networks impaired by the loss of CX3CR1 cause changes in the spatiotemporal inputs of chemokine signaling to osteoblastic cells, which may lead to the temporally disordered expression of osteogenic transcription factors and bone matrix proteins, thus resulting in impaired mineral deposition.
The roles of the CX3CR1–CX3CL1 axis in the maintenance of osteoclast precursors
The osteoclast dysfunction resulting from CX3CR1 deficiency could be largely associated with diminished signaling along the RANK–RANKL axis. The downregulation of both Rank and Rankl, and the upregulation of Osteoprotegerin, were observed in the bone tissue of Cx3cr1-deficient mice (Fig. 2D).
Cultured osteoblastic cells isolated from Cx3cr1-deficient mice exhibited remarkable reductions in the Rankl expression level (Fig. 3C). Co-cultures of wild-type pre-osteoclasts with osteoblastic cells from Cx3cr1-deficient mice failed to induce TRAP-positive osteoclasts (Fig. 3C), confirming the presence of a functional reduction in the osteoclast-supporting activity in Cx3cr1-deficient osteoblastic cells, most likely due to the downregulation of Rankl. Furthermore, in Cx3cr1-deficient osteoclasts, the levels of Rank and other osteoclastic markers were decreased, while the levels of myeloid-lineage markers were increased (Fig. 6B). These differences in the expression of various markers and functions in Cx3cr1-deficient osteoclasts compared to those in wild-type cells could be due to functional changes in the differentiation potential of these cells prior to the culture. Given that no detectable level of Cx3cl1 was expressed in the osteoclast lineage cells (Koizumi et al., 2009) and that the expression of Cx3cr1 in wild-type mouse-derived osteoclastic cells was readily downregulated to the basal level after RANKL stimulation (Fig. 5A), the physiological interaction between CX3CL1 and CX3CR1 possibly occurs prior to, and/or concomitantly with, the initial RANK–RANKL interaction to induce osteoclastogenesis in the bone marrow environment where other type of cells, such as endothelial cells and osteoblastic cells, express CX3CL1 (Bazan et al., 1997; Koizumi et al., 2009). Indeed, our flow cytometric analysis of bone marrow cells after M-CSF and RANKL stimulation demonstrated that there was a slight increase in the number of myeloid precursors, but a significant decrease in osteoclastic precursors (R2 gated cells) with lower RANK expression in Cx3cr1-deficient cells (Fig. 7D; Table 1), strongly suggesting a critical role for Cx3cl1 in the regulation of osteoclast precursor populations.
Consistent with these ideas regarding the roles of the CX3CR1–CX3CL1 axis in the osteoclast precursor and immature osteoclast stages, treatment of the osteoclastic cells with rmCX3CL1 prior to RANKL stimulation led to significant downregulation of osteoclastic markers, while the myeloid-lineage markers were upregulated (Fig. 8A,). However, no obvious changes in either osteoclastic or myeloid-lineage markers were observed when this treatment was performed after RANKL stimulation on day 4 (Fig. 8B). These findings regarding the distinct timing of CX3CL1 treatment suggest a role for the CX3CR1–CX3CL1 axis in sustaining osteoclastic precursors, with a smaller contribution to the differentiation of mature osteoclasts. Collectively, our current findings suggest that the CX3CR1–CX3CL1 axis plays a relevant role in the maintenance of osteoclastic precursors, which may have favorable roles in the initial attraction and the subsequent adhesion of osteoclast precursors by osteoblasts in the bone marrow environment, as previously reported by Koizumi et al. (Koizumi et al., 2009).
The osteoclastic phenotypes in CX3CR1 deficiency are very similar to those associated with CCR1 deficiency, which we reported in a previous study (Hoshino et al., 2010). In fact, the Ccr1 expression was dramatically suppressed in Cx3cr1-deficient bones and was significantly reduced in Cx3cr1-deficient osteoclasts (Fig. 2E; Fig. 7B). However, some aspects of the osteoclast phenotypes in Cx3cr1-deficient cells exhibit distinct functions from those of the Ccr1-deficient osteoclasts. First, the Cx3cr1-deficient osteoclasts exhibited obvious actin ring formation, indicating that they have the ability to undergo cell fusion, which was not observed in the Ccr1-deficient cells (Hoshino et al., 2010). Second, the pit formation assay and zymography showed that Cx3cr1-deficient osteoclasts exert obvious mineral resorption abilities; however, the collagen digestion by Cx3cr1-deficient osteoclasts is partially abrogated (Fig. 6C,D), while Ccr1-deficient osteoclasts do not show obvious mineral resorption or collagen digestion (Hoshino et al., 2010).
A possible reason for these phenotypic differences between Cx3cr1- and Ccr1-deficient osteoclasts could be their distinct roles in osteoclastic precursors. A population analysis of the bone marrow cells in Ccr1-deficient mice after RANKL stimulation exhibited significant downregulation of CD11b+CD115+ osteoclastic precursors, while the same analysis of Cx3cr1-deficient mice showed a significant decrease only in the CD11blo (R2 gated) subpopulation (Table 1).
Given the distinct temporal expression patterns and functions of CCR1 (Hoshino et al., 2010) and CX3CR1 in this work, the CCR1-mediated axis appears to function in a wider range of activities during the course of osteoclast differentiation than does the CX3CR1 axis. CCL5 and CCL9 are critical ligands for CCR1 in bone cells, and are activated in differentiated osteoclasts (Hoshino et al., 2010). Simultaneous blockade with neutralizing antibodies against CCL5 and CCL9 inhibited osteoclast formation to a comparable level to that by PTX treatment (Hoshino et al., 2010), therefore, it is likely that they are major chemokine ligands that transduce Gαi protein-mediated signals for osteoclastogenesis. In Ccr1-deficient osteoclasts, both Ccl5 and Ccl9 were significantly suppressed (Hoshino et al., 2010), while significant upregulation of Ccl9 and partial reduction of Ccr1 were observed in the corresponding Cx3cr1-deficient cells (Fig. 7B,C), which could lead a partial breakdown of the CCR1 axis during osteoclast differentiation and may cause a milder phenotype in terms of the osteoclast function in the Cx3cr1-deficient mice.
In conclusion, the present observations provide further evidence for the physiological roles of the CX3CR1–CX3CL1 axis in bone metabolism, including the functional differentiation of both osteoblasts and osteoclasts, through different modes of the CCR1-mediated axis. Our current findings emphasize the relevance of the CX3CR1–CX3CL1 axis as a therapeutic target for diseases associated with bone destruction, since this chemokine axis appears to play a pivotal role in the chemokine networks involved in bone metabolism. Further studies are needed to evaluate the potential of targeting this axis for therapy.
Materials and Methods
Mice
Standard C57BL/6 mice (6–9-week-old, male) were obtained from CLEA Japan. Cx3cr1-deficient mice (Niess et al., 2005) were purchased from Jackson laboratories and backcrossed for eight to ten generations on the C57BL/6 background. These mice were bred and maintained under pathogen-free conditions at the animal facilities of the University of Tokyo.
Laboratory animal care and experiments
All experiments were performed according to the Institutional Guidelines for the Care and Use of Laboratory Animals in Research and with the approval of the local ethics committees of the University of Tokyo, the Research Institute of International Medical Center of Japan and Tokyo Medical and Dental University.
Reagents
Recombinant murine M-CSF and RANKL were purchased from R&D Systems Inc. (Minneapolis, MN, USA) and PeproTech Inc. (Rocky Hill, NJ, USA), respectively. The recombinant soluble form of mouse CX3CL1/fractalkine (rmCX3CL1) was purchased from R&D Systems. Hamster anti-CX3CL1 neutralizing antibodies (anti-CX3CL1 neuAb) and control hamster IgG were provided by Dr Toshio Imai (Kan Research Institute, Kobe, Japan). Specific antibodies for murine CX3CR1 and CX3CL1 were purchased from Abcam (Cambridge, MA).
Peripheral quantitative computed tomography and microcomputed tomography
The bone scores were measured with peripheral Quantitative Computed Tomography (pQCT) using the XCT Research SA+ system (Stratec Medizintechnik GmbH, Pforzheim, Germany), as described previously (Hoshino et al., 2010). The scores were defined according to the American Society for Bone and Mineral Research standards (Hildebrand et al., 1999). The microstructure parameters were three-dimensionally calculated as described previously (Ito et al., 2005).
Bone histomorphometry
Bone histomorphometry was performerd as previously described (Hoshino et al., 2010). The nomenclature, symbols and units used in the present study are those recommended by the Nomenclature Committee of the American Society for Bone and Mineral Research (Parfitt et al., 1987).
Cell culture of bone-marrow-derived osteoclasts and osteoblastic cells
Murine bone marrow cells cultured in α-MEM were used as the sources of osteoclastic and osteoblastic cell cultures as previously described (Hoshino et al., 2010). In these cultures, the non-adherent cells were collected for bone-marrow-derived macrophages and osteoclastic cells, and adherent bone mesenchymal stromal cells were collected for osteoblastic cells. To generate pre-osteoclasts, non-adherent cells were passed through a column filled with Sephadex G-10 microspheres (Amersham Biosciences, Piscataway, NJ), and the cells were then cultured with 10 ng/ml M-CSF and 20 ng/ml RANKL for 4 days. The contamination of stromal/osteoblastic cells was monitored by an RT-PCR analysis, as a low expression level of the Osteoprotegerin gene indicates the presence of stromal/osteoblastic cells (Hoshino et al., 2010). For the differentiation analysis in the presence of rmCX3CL1, bone marrow cells were stimulated with M-CSF and RANKL (day 1 to day 10) in the presence or absence of rmCX3CL1 (50 ng/ml). The culture media were replaced every three days.
Osteoblastic differentiation in adherent bone marrow mesenchymal stromal cells was induced by culture in α-MEM containing osteogenic factors (10% FBS, 200 µM ascorbic acid, 10 mM β-glycerophosphate and 10 nM dexamethasone). The culture media was replaced once every 3 days. The mineral deposition was evaluated using von Kossa's method (Polysciences, Inc., Warrington, PA). The calcium content was quantified using the Calcium E-test from WAKO (Wako Chemicals, Osaka, Japan), and the results were normalized using the DNA content of the lysates.
Co-culture experiments with osteoclast precursors and osteoblasts were performed by inoculating bone-marrow-derived precursors (1×105 cells/well) onto a layer of osteoblastic cells that had been cultured for 21 days with osteoblast-inducing media in 24-well plates as previously described (Hoshino et al., 2010). The bone resorption activity of the co-culture studies were also conducted using bone slices as described previously (Hoshino et al., 2010).
Immunohistochemical staining
Immunohistochemical staining of the tibiae dissected from 4-week-old C57BL/6 mice was conducted as previously described (Watanabe et al., 2012). Paraffin-embedded sections of 5 µm were stained with specific antibodies against CX3CR1 and CX3CL1 (Abcam, Cambridge, MA), followed by Alexa Fluor 568 antibodies (Molecular Probes, Life Technologies, Grand Island, NY), and were counterstained with DAPI (DOJINDO Laboratories, Kumamoto, Japan).
The osteoblastic cell line, MC3T3-E1 (RIKEN BOCC, Tsukuba, Japan), was maintained and cultured as previously described (Watanabe et al., 2012). Cells were seeded on 2-well culture slides (BD Falcon, San Jose, CA) and then fixed with 4% paraformaldehyde 2 and 4 days after culture. Double immunofluorescence staining was sequentially conducted using antibodies against CX3CR1 and CX3CL1, and slides were counterstained with DAPI. Fluorescence images and differential interference contrast (DIC) images were captured using an ECLIPSE Ni-E fluorescence microscope (NIKON, Tokyo, Japan). Image processing was conducted using the NISE Elements software program (NIKON, Tokyo, Japan). Immunohistochemical staining of cultured osteoclasts were carried out as described previously (Hoshino et al., 2010).
Real-time quantitative PCR (RT-PCR) analysis
Total cellular RNA from the cultures of osteoclastic cells, osteoblastic cells and bone tissue sample (the proximal tibia after the removal of bone marrow at the metaphysial regions by flushing) was isolated using the RNeasy kit (Qiagen, Valencia, CA). The total RNA was then reverse-transcribed into cDNA using the Superscript III RT kit (Invitrogen, Carlsbad, CA). A real-time quantitative PCR (RT-PCR) analysis was performed using the ABI 7700 sequence detector system and the Taqman® Gene Expression Analysis software program (Applied Biosystems, Foster City, CA) as described previously (Hoshino et al., 2010).
Measurement of chemokines, TRAP, BALP and NTx
The murine chemokine levels were determined using ELISA for CCL5, MAB463 and BAF463 antibodies (R&D systems). Murine tartrate-resistant acid phosphatase 5b (TRAP5b), BALP and NTx in the serum and culture supernatants were measured using the murine TRAP EIA assay kit (Immunodiagnostic system, Fountain Hills, AZ), the murine BALP ELISA kit (Cusabio Biotech Co Ltd, Wilmington, DE) and the NTx ELISA kit (SRL, Inc., Tokyo, Japan), respectively.
Flow cytometry
Flow cytometric analysis of osteoclast precursors were performed as previously described (Hoshino et al., 2010). Pacific Blue-, FITC-, PE-, APC-, PerCP-Cy5.5-, PE-Cy7-, APC-Cy7 or biotin-conjugated anti-mouse antibodies to CD45.2 (104), CD115 (AFS98), CD265/RANK (R12-31) and subclass-matched control antibodies were purchased from eBioscience (San Diego, CA). Anti-mouse antibodies to FcγR (2.4G2), Ly6C/6G (RB6-8C5), CD11b (M1/70) and CD19 (1D3) were purchased from BD Pharmingen (San Diego, CA).
Statistical analyses
The data are presented as the means ± s.e.m. Statistical significance was determined with a post-hoc test or one-factor factorial ANOVA (Fig. 3C; Fig. 5; Fig. 7A–C; Table 1), Wilcoxon Mann–Whitney (non-parametric analysis, Fig. 2C), Tukey–Kramer HSD test (multiple comparisons, Fig. 3B–D and Fig. 8A,B) and Student's t-test (other figures) using the KaleidaGraph® 4.0 software program for Windows (Synergy Software, Reading, PA, USA). * and # indicate a significant upregulation and downregulation, respectively (P<0.05). NS: not significant.
Acknowledgements
The authors express sincere thanks to Mami Tamai, Satoshi Takiguchi and Norio Ohba at Nikon Instech., Ltd for their expertise on microscopy and image processing.
Funding
This work was supported by a Grant-in-Aid for Scientific Research from the Japan Society for the Promotion of Science [grant KAKENHI to A.H., A.Y. and T. Iimura]; the Naito Foundation to A.H.; the Ministry of Education, Culture, Sports, Science and Technology, Global Center of Excellence Program, ‘International Research Center for Molecular Science in Tooth and Bone Diseases’ to A.Y. and T. Iimura]; the Ministry of Education, Culture, Sports, Science and Technology Grant-in-Aid for Scientific Research on Innovative Areas ‘Fluorescence Live Imaging’ [grant number 22113002 to T. Iimura]; Takeda Science Foundation to T. Iimura; and the Ministry of Health, Labor and Welfare [grant number H19-nano-012 to K.Y.].




![Impairment of osteoblast differentiation in CX3CR1-deficient cells. (A) Osteoblastic cells isolated from wild-type (open bars) and Cx3cr1-deficient mice (filled bars) were cultured. The mineralized nodules were stained using von Kossa's method and the samples were photographed. The number of mineralized nodules was calculated (means ± s.e.m., n = 4), and the calcium content in the nodules was measured and normalized to the DNA content in the lysates (means ± s.e.m., n = 4; right graph). (B) The relative expression levels of transcripts of osteoblastic transcription factors (Runx2 and Osterix) and markers (Balp, Collagen1a1, Osteonectin and Osteocalcin) by immature (day 14, before mineral deposition) or mature (day 21, with mineralization) osteoblastic cells isolated from wild-type (open circle) and Cx3cr1-deficient mice (filled circle) were measured using RT-PCR (means ± s.e.m. n = 8). The statistical significance was determined with the Tukey–Kramer HSD test. * and # indicate a significant upregulation and downregulation, respectively (P<0.05) compared with unstimulated stromal cells (P<0.05). There were significant differences between wild-type and Cx3cr1-deficient cells, with significant upregulation denoted by ⋆ and downregulation by ★, respectively (P<0.05). (C,D) Co-culture of osteoblasts and osteoclasts from wild-type and Cx3cr1-deficient mice. (C) The relative expression levels of Rankl and Osteoprotegerin by the osteoblastic cells derived from wild-type (open circles) and Cx3cr1-deficient mice (filled circles) were measured using RT-PCR (means ± s.e.m., n = 8). (D) Osteoclasts were induced from wild-type osteoclast precursors by co-culture with osteoblasts of wild-type and Cx3cr1-deficient mice. (Left panels) Multinuclear osteoclasts were visualized with TRAP chromogenic stain on osteoblastic cells derived from wild-type and Cx3cr1-deficient mice (magnification ×100). (Right panel) The number of TRAP+ multinuclear osteoclasts was counted (means ± s.e.m., from duplicate experiments, n = 3). Osteoclast culture with M-CSF and RANKL without osteoblasts were carried out as positive controls. #Significant differences from the co-culture of osteoclasts with wild-type osteoblasts, P<0.05. (E) The relative expression levels of Cx3cr1, Cx3cl1 and Ccr1 by the immature and mature osteoblastic cells from wild-type (open circles) and Cx3cr1-deficient mice (filled circles) as measured by RT-PCR (means ± s.e.m., n = 6). The difference between the wild-type and Cx3cr1-deficient cells was statistically significant [downregulation (★), N.D. not detected]. (F) Chemokines (CCL5 and CCL9) in the culture supernatants of wild-type and Cx3cr1-deficient osteoblastic cells were measured using ELISAs (means ± s.e.m., duplicated, n = 4).](https://cob.silverchair-cdn.com/cob/content_public/journal/jcs/126/4/10.1242_jcs.113910/4/m_jcs-126-04-1032-f03.jpeg?Expires=1714477272&Signature=YBJVvfKczU0zlGJcYUjJi9c0bcNVbBxxepzLwGIm4XQ1uRw84C3PaLSYIJ~PpeEN6cM8gOYzVk-jeezqSDcfSFXfLyx9~3nTDlyVZhHAWtY6gvcQBNyzRjbWCVv4lHseqTcAdYZFWdswM5PNf-gzrY6gBJlHm28XYLaH6H8qUfVN74SvgV6aiDZNKlr4RmsKMnGerZhZ8myTl-jEfUAGX03dUSuRK8feZCzu7~7A6pgZmv2JGYOWU~g68Qk4ezG855dLnWJBs8Q0qZPvUfcmfp86KSPewecNOJv0FTmcf20rsOWhJLJitt77wezJFz2ots6NOFvO5xVVK4RZrx~F8w__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)


![Impairment of osteoclast functions by CX3CR1 deficiency. (A), Osteoclastic cells were induced from the bone marrow of wild-type and Cx3cr1-deficient mice using M-CSF and RANKL treatment. In vitro osteoclast cultures from wild-type and Cx3cr1-deficient precursors were carried out for 10 days (upper panels) or 17 days (lower panels) and cultures were stained with an anti-CathepsinK polyclonal antibody (red), and for F-actin (green) and nuclei (blue). Scale bar: 50 µm. (B) The relative expression levels of transcripts of osteoclastic differentiation markers on day 4 after culture[RANK and its downstream transcription factor NFATC1; bone-specific enzymes, TRAP5B and CathepsinK protease; osteoclast-specific integrins alphaV and beta3; and myeloid-lineage cell markers S1P1 and IRF-8] in wild-type (open bars) and Cx3cr1-deficient (filled bars) preosteoclasts were measured by RT-PCR (means ± s.e.m., n = 5). *Significantly upregulated, #significantly downregulated compared with wild-type controls, P<0.05. (C) Scanning electron micrographs of the pit formation assay of wild-type and Cx3cr1-deficient osteoclasts. Scale bar: 2 µm. (D) The collagen digestion activity of wild-type and Cx3cr1-deficient osteoclasts was measured using collagen-based zymography. BMM, cell lysates from bone-marrow-derived macrophages (10 µg protein/lane); WT and KO, wild-type and Cx3cr1-deficient osteoclast lysates (1 and 10 µg protein/lane), respectively.](https://cob.silverchair-cdn.com/cob/content_public/journal/jcs/126/4/10.1242_jcs.113910/4/m_jcs-126-04-1032-f06.jpeg?Expires=1714477272&Signature=osMCbvFbNKUnlZ-kPdBbQBrdk03pnpLxAA7ZlLyfsRp6tGVXi5n1JdAUb79~UyH09T8i7tjOfgGfl6DU8SYji9UUOv2UDEfhauBFTvHuYNZ-7Vtipj33ZzAe1d3VVD4tXXbnjkormmF~jPtT5RwEwO0gfYfuCv42NCKV3pr2f-JO7lTvjee64K4ihn5IxB7K90QvAAAM9lHP3W5~L625l8N3Q7KTe-xM8e6I5UD47parn~PIxZWbbPrIB0Ju-pFX1XkR7SriwrCJbxFy1wDXTKdClL1PYbLpHAIwXHunYv0OCPsjZjSLCn0iZNpo7eueBeZNgAuCgHIjfn7OujMpqg__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)