Impairment of the gut epithelial barrier by agents such as IFNγ may play a key role in the pathogenesis of inflammatory disorders by increasing the paracellular penetration of luminal macromolecules, potentially including bacterial antigens. Owing to limitations of current paracellular probes, little is known about the precise functional changes induced by IFNγ and how these relate to the development of increased macromolecular permeability. Here we investigate how IFNγ modulates this pathway in T84 monolayers using a novel profiling technique that resolves different populations of paracellular pores by simultaneous analysis of 24 permeability probes of defined molecular size. Two types of functional pore present in control monolayers, an abundant restrictive pore with a radius of ∼4.5 Å and a much larger but infrequent, non-restrictive pore, were differentially regulated by IFNγ. Incubation with IFNγ dose-dependently and reversibly increased the frequency of the non-restrictive pores while having no significant effect on the restrictive component. Cytokine-induced increases in β, the descriptor of the non-restrictive pore, correlated closely with increased permeability to large molecules (10 kDa) including E. coli-derived lipopolysaccharide, but not small (0.182 kDa) molecules. This effect was associated with changes in expression of the tight junction proteins occludin and claudin-1. These data suggest that IFNγ selectively increases the transepithelial flux of large molecules by activating specific pathways within the junctional pore. One hypothesis is that this process may be activated in the early stages of the inflammatory response, facilitating the passage of large and potentially antigenic molecules across the gut without gross disruption of the barrier to small molecules.
Introduction
Under normal circumstances, the immense load of bacteria and associated antigens present in the lumen of the lower small intestine and colon is effectively contained by the intestinal epithelium. According to the `leaky gut' theory of intestinal disease, an initial injury- or inflammatory-mediated insult causes disruption of tight junctions and increased paracellular permeability allowing entry of luminal antigens (Hollander, 1999; Clayburgh et al., 2004). The resulting immune activation triggers repeat cycles of inflammatory response and barrier disruption that establish and propagate inflammatory bowel disease.
Evidence from both cultured cell and animal models suggests that the pro-inflammatory cytokine, interferon-γ (IFNγ) may act as a key modulator of intestinal barrier function (Walsh et al., 2000; Ferrier et al., 2003). Incubation of colonic epithelial cell monolayers with IFNγ alone (Madara and Stafford, 1989; Youakim and Ahdieh, 1999) or in combination with other cytokines (Han et al., 2003; Bruewer et al., 2003) elicits dramatic reductions in transepithelial resistance (TER) along with increased solute permeability. These effects are mediated at the molecular level by altered expression and/or redistribution of tight junction proteins and perturbations of the actin cytoskeleton (Youakim and Ahdieh, 1999; Bruewer et al., 2003). Recent evidence suggests that IFNγ-mediated inhibition of epithelial Na+,K+-ATPase activity plays a critical role in initiating the signalling pathways that lead to barrier disruption (Sugi et al., 2001; Bertelsen et al., 2004). Despite these studies, our understanding of how IFNγ modulates the paracellular pore at the functional level, and how this might affect intestinal permeability to antigens, remains limited. One unresolved question is whether this cytokine causes non-specific disruption of tight junctions or elicits more subtle effects on junctional permeability to facilitate antigen entry.
There is an increasing realisation that the molecular complexity of tight junctions (D'Atri and Citi, 2002; Rahner et al., 2001) may be the basis for a functional complexity involving multiple populations of size- and charge-limiting pores that could allow different physiological stimuli to induce specific effects on paracellular permeability (Karczewski and Groot, 2000). However, the poor resolution and sensitivity inherent in conventional approaches to measuring paracellular function have limited our ability to identify functional heterogeneity. We have recently described a functional profiling technique that simultaneously measures the transepithelial permeability of 24 PEG oligomers of defined molecular radius by mass spectrometry (Watson et al., 2001). When analysed by a modified sieving model, this approach resolves distinct populations of paracellular pores in colonic epithelial cells that appear to be differentially regulated by tight junction modulators such as EGTA and sodium caprate (Watson et al., 2001). The aim of the present study was to utilise this approach to provide a detailed insight into the functional modulation of the paracellular route by IFNγ in gut epithelial cells.
Materials and Methods
Materials
Recombinant human IFNγ (104 IU/μg) was purchased from R&D Systems, Abingdon, UK. Monoclonal anti-occludin (OC-3F10), polyclonal anti-claudin-1, anti-claudin-2 and anti-claudin-3 antibodies were from Zymed Laboratories, San Francisco, USA. Goat anti-mouse and anti-rabbit horseradish peroxidase (HRP)-conjugated antibodies were purchased from Bio-Rad, Hemel Hempstead, UK. Fluorescein isothiocyanate (FITC)-labelled E. coli lipopolysaccharide was obtained from Sigma-Aldrich, Poole, UK. [14C]mannitol (56 mCi/mmol) was purchased from Amersham International, Chalfont St Giles, UK. FITC-labelled 10 kDa dextran (FD10) and Rhodamine-labelled, lysine-fixable 10 kDa dextran were from Molecular Probes Europe, Leiden, Netherlands. All other chemicals including PEG400, PEG1000, filipin, LY29-4002 and chlorpromazine were obtained from Sigma-Aldrich, Poole, UK.
T84 cell culture
T84 cells (passages 98-120) were maintained in a 1:1 mixture of Dulbecco's modified Eagle's medium (DMEM) and Ham's F12 medium supplemented with 14 mM NaHCO3, 50 IU penicillin and 50 μg/ml streptomycin in 25cm2 flasks at 37°C in a 5% CO2 constant humidity environment with medium replaced three times a week. For transport experiments and immunoblot analysis, cells were seeded on 0.4 μm pore size Snapwell or Transwell culture inserts respectively (Costar, High Wycombe, UK). Inserts were seeded with 2-3×105 cells/cm2 and were grown for at least 21 days before use in experiments, to allow development of monolayers with a high (>1200 Ω ·cm2) and stable transepithelial resistance (TER). Development of TER was monitored using an Evometer (World Precision Instruments) fitted with chopstick electrodes.
Treatment with IFNγ
T84 monolayers were exposed to IFNγ at various concentrations (0.01-10 ng/ml) on the basolateral surface for 4-48 hours in culture medium. Changes in TER were monitored throughout using the Evometer. At the end of this period, culture medium was removed, the cells were washed with HBSS at 37°C and either mounted in Ussing chambers for transport studies or processed for immunoblotting of tight junction proteins. In some instances, cells were allowed to recover from IFNγ treatment by washing three times in medium followed by maintenance in complete culture medium without IFNγ for the specified times.
Transport studies
T84 monolayers were removed from the growth medium and washed twice in prewarmed HBSS (supplemented with 20 mM HEPES). Monolayers were subsequently placed in a modified Ussing chamber (1.0 cm2 diffusion window) and equilibrated with HBSS on both apical and basolateral surfaces. Chambers were maintained at 37°C and under constant O2. Spontaneous tissue potential difference (PD) and TER, measured as deflection in PD caused by a 100 μA current pulse, were monitored throughout the experiment. After the equilibration period the paracellular markers PEG400/1000 (2 μg/ml), [14C]mannitol (0.2 μCi/ml; 100 μM), 10 kDa FITC-dextran (10 μM; FD10) were added to the apical (donor) chamber. A 100 μl sample was removed from the donor chamber to determine the initial concentration. Samples were removed from the receiver chamber at 30 minute intervals and replaced with fresh buffer. Permeability to bacterial lipopolysaccharide was assessed by adding FITC-LPS (0.2 mg/ml from Escherichia coli 0111:B4) to the apical chamber and the basolateral medium sampled after 4 hours. Concentrations of mannitol were assessed by liquid scintillation counting and FD10 and FITC-LPS by fluorimetry (excitation 485 nm/emission 530 nm) respectively. PEG samples were stored at –70°C until analysed by LC-MS. The detailed protocol for resolution of PEG oligomers by LC-MS has been described previously (Watson et al., 2001).
Mathematical modelling of paracellular permeation
The resolution of the polydisperse mixture of PEG 400/1000 by LC-MS allows the paracellular permeability of 24 polyethylene glycols of increasing molecular mass (0.238-1.25 kDa) and molecular radius (3.5-7.4 Å) to be measured simultaneously. These data provide a profile of paracellular permeability over a range of molecular sizes that can be modelled using a modified sieving model (Watson et al., 2001).
Internalisation studies
To investigate the possible effects of IFNγ on probe internalisation, control or IFNγ-treated (10 ng/ml; 48 hours) monolayers were equilibrated in HBSS and incubated on the apical surface with HBSS containing 1 mg/ml Rhodamine-labelled, lysine-fixable 10 kDa dextran for 60 minutes at 37°C under conditions which replicated the permeability studies using FITC-dextran. At the end of this period, monolayers were washed three times with HBSS at 4°C, fixed with 4% paraformaldehyde and permeabilised with 0.1% Triton X-100. After washing with PBS, all samples were stained with the nuclear stain DAPI (4′,6-diamidino-2-phenylindole dihydrochloride; 0.2% in PBS) for 5 minutes at 4°C, followed by further washing in PBS and mounting on slides with Vectashield (Vector Laboratories, Peterborough, UK). Studies of the effect of extracellular calcium depletion on dextran internalisation used a modification of the method of Ivanov et al. (Ivanov et al., 2004). Monolayers were washed repeatedly in calcium-free Eagle's minimal essential medium for suspension culture (S-MEM; Gibco) supplemented with 2 mM EGTA, 10 mM HEPES, 14 mM NaHCO3 and 50 IU penicillin/50 μg/ml streptomycin and 10% foetal calf serum at 4°C. One mg/ml Rhodamine-dextran in pre-warmed S-MEM was then placed on both apical and basolateral surfaces and the monolayers incubated for 120 minutes at 37°C. Monolayers were subsequently washed, fixed and permeabilised as described above.
Stained monolayers were analysed by confocal laser-scanning microscopy on a Biorad MRC1024 confocal system mounted on a Nikon Eclipse TE300 fluorescence microscope with a X40 Plan Fluor oil objective. Images shown are representative of three similar monolayers with multiple images taken from each preparation.
In other studies, control and IFNγ-treated (10 ng/ml) monolayers were incubated on the apical surface with HBSS containing 14C-PEG4000 (1 μCi/ml) for 60 minutes. At the end of the incubation, the radio-labelled PEG4000 was removed and the monolayers washed three times rapidly in an excess of ice-cold HBSS. Washed monolayers were placed in an emulsifying cocktail (Ultima Gold, Perkin-Elmer, Beaconsfield, UK) for scintillation counting.
Immunoblotting of tight junction proteins
T84 monolayers were lysed at 4°C by scraping into a buffer containing 120 mM NaCl, 25 mM HEPES (pH 7.5), 2 mM EDTA, 25 mM NaF, 1 mM NaVO4, 1% (w/v) Triton X-100 and 5% (v/v) protease inhibitor cocktail (Sigma). Samples were left on ice for 30 minutes after which detergent-insoluble material was pelleted by centrifugation at 12,000 g for 30 minutes at 4°C. The supernatant (detergent-soluble fraction) was retained. The detergent-insoluble pellet was solubilised in a buffer containing 25 mM HEPES (pH 7.5), 2 mM EDTA, 25 mM NaF, 1 mM NaVO4, 5% (v/v) protease inhibitor cocktail and 1% (w/v) sodium dodecyl sulphate (SDS) by sonication for 3 seconds on ice. The protein content of both detergent soluble and insoluble fractions was determined by the BCA method (Pierce, USA). Fractions were stored at –80°C until use.
Detergent soluble and insoluble fractions (20 μg/well) were separated by SDS-PAGE on either 7.5% (occludin) or 12% (claudin) polyacrylamide gels. After electrophoretic transfer to nitrocellulose membranes (Hybond), membranes were blocked at 4°C overnight in TBS-T (50 mM Tris-HCl pH 7.9, 150 mM NaCl and 0.05% v/v Tween 20) containing 2% (w/v) milk protein. Membranes were washed in TBS-T and probed with polyclonal antibodies to claudin-1, claudin-2 or claudin-3 or a monoclonal antibody to occludin (all at 1:1000 dilution in TBS-T) for 1 hour. After washing and incubation with the appropriate horseradish peroxidase-conjugated secondary antibody (1:5000), protein bands were visualised using the ECL system (Amersham Pharmacia, Bucks, UK) followed by exposure of blots to X-OMAT film (Kodak-Eastman). Where indicated, immunoblot images were scanned and quantified densitometrically using Scion Image software (Scion Corporation, Frederick, USA). In all cases, membranes were also stained with Coomassie Blue to verify equal protein loading in each well.
Statistical analysis
Results are expressed as means±s.e.m. for the indicated number of observations (n). Data were analysed by ANOVA with post hoc Bonferroni or paired t-tests as appropriate. A P value of ≤0.05 was accepted as the level of statistical significance. All analyses were undertaken using Graphpad Prism software (Graphpad Prism, San Diego, California, USA).
Results
Incubation of T84 monolayers with IFNγ for 48 hours induced a dose-dependent reduction in TER (Fig. 1A) of >90% at 10 ng/ml with half maximal effects at ∼0.3 ng/ml. This was accompanied by marked changes in the permeability of PEG oligomers of increasing molecular size (Fig. 1B). In control monolayers, PEG permeability exhibits a biphasic profile similar to that described previously (Watson et al., 2001) with a restrictive component with a sharp molecular size `cut-off' and a second component that is not restrictive for these size molecules (i.e. up to at least 7.39 Å). Increasing concentrations of IFNγ produced a progressive upward shift in T84 PEG permeability while maintaining an essentially biphasic profile (Fig. 1B). However, closer examination of the data shows that the increases in PEG permeability do not occur to the same extent across the whole molecular size range but are much more pronounced for larger oligomers being 2.7-fold (3.7±0.13×10–6 compared to 1.35±0.11×10–6 cm/second; P<0.01) and 15-fold (0.82±0.04 compared to 0.054±0.006; P<0.01) increase in permeability for PEG 238 and PEG 1250 respectively).
Concentration-dependent effects of IFNγ on PEG oligomer permeability and TER in T84 monolayers. After a 48-hour incubation with IFNγ, monolayers were mounted in modified Ussing chambers in HBSS. (A) Decrease in TER in response to basolateral IFNγ at concentrations of 0.01-10 ng/ml for 48 hours. (B) Apical to basolateral permeability profiles of PEG oligomers of increasing molecular mass (0.238-1.25 kDa) and molecular radius (3.5-7.4 Å) following a 48-hour incubation with 10 ng/ml (▪); 1 ng/ml (•) and 0.1 ng/ml (▴) IFNγ or vehicle (□). Permeability data is the mean of six 30-minute flux periods. Data shown are expressed as mean±s.e.m. of four monolayers in each group.
Concentration-dependent effects of IFNγ on PEG oligomer permeability and TER in T84 monolayers. After a 48-hour incubation with IFNγ, monolayers were mounted in modified Ussing chambers in HBSS. (A) Decrease in TER in response to basolateral IFNγ at concentrations of 0.01-10 ng/ml for 48 hours. (B) Apical to basolateral permeability profiles of PEG oligomers of increasing molecular mass (0.238-1.25 kDa) and molecular radius (3.5-7.4 Å) following a 48-hour incubation with 10 ng/ml (▪); 1 ng/ml (•) and 0.1 ng/ml (▴) IFNγ or vehicle (□). Permeability data is the mean of six 30-minute flux periods. Data shown are expressed as mean±s.e.m. of four monolayers in each group.
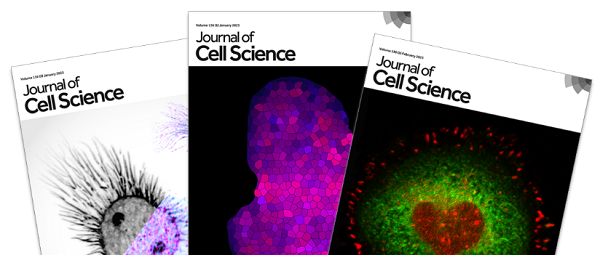
The IFNγ-induced changes in PEG permeability were further analysed using the two-component sieving model (Table 1). This provides further evidence that the primary effect of the cytokine is a preferential increase in the paracellular permeability to larger molecules. Values for both rsl, an estimate of the diameter of the restrictive pore and α, which is proportional to the number of restrictive pores were unchanged in IFNγ-treated monolayers. In contrast, values for β, the descriptor of the non-restrictive component of PEG flux increased markedly, being 15-fold higher in cells exposed to 10 ng/ml IFNγ for 48 hours. Fig. 2 compares changes in α and β with the increase in permeability of a large paracellular probe, 10 kDa dextran, following treatment of T84 cells with IFNγ. Values for α show no significant change in response to IFNγ even at concentrations up to 100 ng/ml, whereas β values increase dramatically (Fig. 2A). These effects were accompanied by a marked increase in permeability of the 10 kDa paracellular probe FD10 (Fig. 2B). Indeed, there was a strong correlation between changes in β and FD10 permeability (coefficient of determination r2=0.913; P<0.05) with similar fold increases (15- and 21-fold respectively). The EC50 values for IFNγ activation of these two parameters were also similar (3.6 and 2.2 ng/ml respectively). Changes in β also appeared to be associated with the IFNγ-induced decrease in TER (compare Fig. 2A and Fig. 1A), however, linear regression analysis did not show a statistically significant correlation between these two parameters (r2=0.817; P>0.05). This suggests that increases in the non-restrictive component of PEG flux rather than changes in the size or frequency of the restrictive paracellular pore are responsible for increased permeability to large molecules. The differential effect of IFNγ on the permeability of FD10 compared to the much smaller paracellular probe mannitol provides further support for this hypothesis (Fig. 3).
Effects of IFNγ on the sieving parameters derived from application of the modified sieving model to PEG oligomer permeability across T84 monolayers presented inFig. 1
| . | rs1 (Å) . | α (second-1) . | β (cm2/second) . |
|---|---|---|---|
| Control | 4.3±0.1 | 6.4±0.9 | 0.4±0.1 |
| IFNγ 0.1 ng/ml | 4.5±0.1 (ns) | 6.2±1.1 (ns) | 1.0±0.1 (*) |
| IFNγ 1.0 ng/ml | 4.5±0.2 (ns) | 4.3±0.6 (ns) | 3.5±0.5 (**) |
| IFNγ 10 ng/ml | 4.6±0.5 (ns) | 4.6±0.3 (ns) | 6.1±1.1 (**) |
| 96 hours after IFNγ | 4.3±0.14 (ns) | 5.2±1.1 (ns) | 1.0±0.1 (*) |
| . | rs1 (Å) . | α (second-1) . | β (cm2/second) . |
|---|---|---|---|
| Control | 4.3±0.1 | 6.4±0.9 | 0.4±0.1 |
| IFNγ 0.1 ng/ml | 4.5±0.1 (ns) | 6.2±1.1 (ns) | 1.0±0.1 (*) |
| IFNγ 1.0 ng/ml | 4.5±0.2 (ns) | 4.3±0.6 (ns) | 3.5±0.5 (**) |
| IFNγ 10 ng/ml | 4.6±0.5 (ns) | 4.6±0.3 (ns) | 6.1±1.1 (**) |
| 96 hours after IFNγ | 4.3±0.14 (ns) | 5.2±1.1 (ns) | 1.0±0.1 (*) |
Descriptors of the restrictive and non-restrictive pores (rs1, α and β) are defined in Materials and Methods. Also shown are the sieving parameters for monolayers in which PEG oligomer permeability was measured 96 hours after removal of 10 ng/ml IFNγ. Data are mean±s.e.m. of four separate profiles in each group. Significant differences indicated at *P<0.05 and **P<0.01 compared to levels in the controls; ns, P>0.05 compared to control levels.
One possibility to be excluded was that the selective increase in permeability of larger molecules was due to IFNγ increasing their internalisation and transcellular passage across the monolayers. To address this, intracellular levels of dextran were imaged by confocal microscopy in control and IFNγ-treated (10 ng/ml) monolayers following incubation on the apical surface with lysine-fixable, Rhodamine-labelled 10 kDa dextran under the same conditions as used in the permeability studies (Fig. 4). Small but significant levels of Rhodamine-dextran are found within the cells of the monolayers after 60 minutes of incubation (Fig. 4A) but there was no evidence for an increase in intracellular dextran following IFNγ treatment (Fig. 4B). As a positive control, monolayers were also incubated under a condition that depletes extracellular Ca2+, which has been shown previously to stimulate endocytic activity in T84 cells (Ivanov et al., 2004). This treatment caused a marked increase in intracellular Rhodamine-dextran staining (Fig. 4C).
Correlation of IFNγ-induced changes in the non-restrictive pore descriptor β with increases in permeability of FD10. (A) Changes in the values of the restrictive (α) and non-restrictive (β) pore descriptors calculated from the PEG oligomer permeability profile as described in the Materials and Methods following incubation of T84 monolayers with IFNγ (0-100 ng/ml) for 48 hours. (B) Apparent permeability (Papp) of 10 kDa fluorescent dextran (FD10) measured under the same conditions. Data are expressed as mean±s.e.m. of n=4-6 monolayers in each group. Significant differences in Papp were observed; **P<0.01; *P<0.05 compared with control as indicated.
Correlation of IFNγ-induced changes in the non-restrictive pore descriptor β with increases in permeability of FD10. (A) Changes in the values of the restrictive (α) and non-restrictive (β) pore descriptors calculated from the PEG oligomer permeability profile as described in the Materials and Methods following incubation of T84 monolayers with IFNγ (0-100 ng/ml) for 48 hours. (B) Apparent permeability (Papp) of 10 kDa fluorescent dextran (FD10) measured under the same conditions. Data are expressed as mean±s.e.m. of n=4-6 monolayers in each group. Significant differences in Papp were observed; **P<0.01; *P<0.05 compared with control as indicated.
Incubation of T84 monolayers for 60 minutes with 14C-PEG4000 followed by rapid washing and analysis of cell-associated radioactivity also showed no significant difference between control and IFNγ-treated (10 ng/ml) cells (Control: 0.018±0.002, compared to IFNγ (10 ng/ml): 0.014±0.004% total 14C-PEG per 106 cells; n=3). Taken together these studies suggest that increased internalisation and transcellular passage are unlikely to be a significant factor in the 15- and 21-fold increases in the transepithelial permeability of PEG 1250 and dextran 10 kDa probes respectively, that follow exposure to IFNγ. We next investigated whether the selective opening of a paracellular route for large molecules by IFNγ is associated with an increased passage of antigenic macromolecules such as endotoxin. Untreated T84 monolayers showed a low level of FITC-LPS permeability, which was increased by almost tenfold (P<0.01) following exposure to 10 ng/ml IFNγ (Fig. 5A). This effect followed IFNγ-mediated changes in TER and was also insensitive to inhibitors of transcytotic pathways (Fig. 5B). Chlorpromazine (CPZ) an inhibitor of clathrin-mediated endocytic processes, LY-294002, an inhibitor of PI-3 kinase-mediated macropinocytosis and filipin, an inhibitor of lipid raft-mediated processes had no significant effect on the IFNγ-mediated increase in FITC-LPS. At the concentrations used, these inhibitors had no effect on basal TER, however, higher concentrations of CPZ (20 μg/ml) and LY-294002 (25 μM) caused a reduction in TER and further increased flux of FITC-LPS (data not shown). These data are consistent with IFNγ activating a paracellular route for the passage of large, potentially antigenic, molecules like LPS.
Influence of IFNγ on mannitol and FD10 permeability across T84 monolayers. Following incubation with IFNγ-(0-10 ng/ml) for 48 hours, T84 monolayers were washed with HBSS and mounted in Ussing chambers. 100 μM [14C]mannitol or 10 μM FD10 (final concentrations) were added to the apical chamber and samples removed every 30 minutes for 3 hours for analysis of probe permeation. Results are shown as fold increase in permeability of mannitol and FD10 above control. Papp values for mannitol and FD10 in control monolayers were 0.53±0.15×10–6 and 0.015±0.005×10–6 cm/second respectively. Data are expressed as mean±s.e.m. of four monolayers in each group. Significant differences in permeability were observed; **P<0.01; *P<0.05 compared with control levels as indicated.
Influence of IFNγ on mannitol and FD10 permeability across T84 monolayers. Following incubation with IFNγ-(0-10 ng/ml) for 48 hours, T84 monolayers were washed with HBSS and mounted in Ussing chambers. 100 μM [14C]mannitol or 10 μM FD10 (final concentrations) were added to the apical chamber and samples removed every 30 minutes for 3 hours for analysis of probe permeation. Results are shown as fold increase in permeability of mannitol and FD10 above control. Papp values for mannitol and FD10 in control monolayers were 0.53±0.15×10–6 and 0.015±0.005×10–6 cm/second respectively. Data are expressed as mean±s.e.m. of four monolayers in each group. Significant differences in permeability were observed; **P<0.01; *P<0.05 compared with control levels as indicated.
Intracellular sequestration of dextran in control and IFNγ treated T84 monolayers. (A) Control, (B) IFNγ -treated (10 ng/ml; 48 hours) and (C) Ca2+-depleted T84 monolayers were incubated with 1 mg/ml Rhodamine-labelled 10 kDa dextran for 60-120 minutes as described in Materials and Methods. After fixation, monolayers were stained with the nuclear stain DAPI and analysed by confocal microscopy (x-z) images. Reconstructed confocal images in the x-z plane showing staining for Rhodamine-dextran, DAPI and merged images of the two stains are shown for each of the three groups. Dextran internalisation increased following Ca2+ depletion (areas of intense staining indicated by arrows) whereas IFNγ-treated monolayers showed no change compared to untreated controls. `F' denotes the position of the Transwell filter, which exhibited high levels of dextran staining in all groups. Bar, 50 μm.
Intracellular sequestration of dextran in control and IFNγ treated T84 monolayers. (A) Control, (B) IFNγ -treated (10 ng/ml; 48 hours) and (C) Ca2+-depleted T84 monolayers were incubated with 1 mg/ml Rhodamine-labelled 10 kDa dextran for 60-120 minutes as described in Materials and Methods. After fixation, monolayers were stained with the nuclear stain DAPI and analysed by confocal microscopy (x-z) images. Reconstructed confocal images in the x-z plane showing staining for Rhodamine-dextran, DAPI and merged images of the two stains are shown for each of the three groups. Dextran internalisation increased following Ca2+ depletion (areas of intense staining indicated by arrows) whereas IFNγ-treated monolayers showed no change compared to untreated controls. `F' denotes the position of the Transwell filter, which exhibited high levels of dextran staining in all groups. Bar, 50 μm.
To investigate further the molecular basis for differential effects of IFNγ on the restrictive and non-restrictive components of paracellular permeability, changes in the expression and localisation of tight junction proteins were studied (Fig. 6). Under control conditions, the transmembrane tight junction protein, occludin was expressed as a 65 kDa band in both soluble and insoluble fractions. However the insoluble pool also contained a heterogeneous mixture of polypeptides of higher molecular mass indicative of hyper-phosphorylated forms of the protein (Nishiyama et al., 2001). IFNγ treatment for 48 hours resulted in a dramatic decrease in the levels of occludin bands of higher molecular mass in the insoluble fraction. This was accompanied by a more modest reduction in the level of the main 65 kDa species. The effects of IFNγ on the expression profile of three claudin species CLD1, CLD2 and CLD3 were markedly different (Fig. 6). Under control conditions, CLD1 was distributed primarily in the soluble fraction with smaller amounts in the insoluble pool. Following exposure to IFNγ, there was a significant increase in the levels of CLD1 associated with the insoluble pool. In contrast, the expression of CLD3 expression did not appear to be influenced by IFNγ and CLD2 was not consistently detected in these cells under either control or IFNγ-stimulated conditions.
Influence of IFNγ on permeability to bacterial lipopolysaccharide. (A) Control or IFNγ-treated T84 monolayers (10 ng/ml; 48 hours), were washed with HBSS and 0.2 mg/ml FITC-LPS added to the apical surface. The flux of FITC-LPS into the basolateral chamber was measured after 4 hours by fluorimetry and shown in μg/hour/cm2 as mean±s.e.m. of five to seven monolayers in each group. (B) Effect of inhibitors of endocytic pathways on FITC-LPS flux. Monolayers were exposed to 10 μg/ml chlorpromazine (CPZ), 10 μM LY-294002 or 3 μg/ml filipin for 15 minutes prior to addition of FITC-LPS. The IFNγ-mediated increase in FITC-LPS flux in the presence of inhibitors was not significantly different to that observed in the absence of inhibitors. Data are mean±s.e.m. of three to six monolayers in each group.
Influence of IFNγ on permeability to bacterial lipopolysaccharide. (A) Control or IFNγ-treated T84 monolayers (10 ng/ml; 48 hours), were washed with HBSS and 0.2 mg/ml FITC-LPS added to the apical surface. The flux of FITC-LPS into the basolateral chamber was measured after 4 hours by fluorimetry and shown in μg/hour/cm2 as mean±s.e.m. of five to seven monolayers in each group. (B) Effect of inhibitors of endocytic pathways on FITC-LPS flux. Monolayers were exposed to 10 μg/ml chlorpromazine (CPZ), 10 μM LY-294002 or 3 μg/ml filipin for 15 minutes prior to addition of FITC-LPS. The IFNγ-mediated increase in FITC-LPS flux in the presence of inhibitors was not significantly different to that observed in the absence of inhibitors. Data are mean±s.e.m. of three to six monolayers in each group.
Differential Triton-X-100 solubility of tight junction proteins and the effect of IFNγ treatment on protein expression. (A) T84 cells were treated for 48 hours with 10 ng/ml IFNγ and then extracted as described in Materials and Methods. Triton-soluble (S) and Triton-insoluble (I) fractions were immunoblotted with antibodies to claudin-1, claudin-2, claudin-3 and occludin. Images are representative of at least three separate experiments. As a positive control for claudin-2, the expression of this protein in untreated Caco-2 monolayers is also shown. (B) Densitometric analyses of immunoblots of claudin-1, occludin (65 kDa) and high molecular mass (phosphorylated) occludin in the insoluble fraction of control and IFNγ-treated T84 monolayers. The graphs show the change in protein levels in IFNγ-treated monolayers as a % of control and are mean data from five separate experiments. Significant differences in protein levels were observed; *P<0.05; **P<0.01 compared with controls as indicated by paired t-test.
Differential Triton-X-100 solubility of tight junction proteins and the effect of IFNγ treatment on protein expression. (A) T84 cells were treated for 48 hours with 10 ng/ml IFNγ and then extracted as described in Materials and Methods. Triton-soluble (S) and Triton-insoluble (I) fractions were immunoblotted with antibodies to claudin-1, claudin-2, claudin-3 and occludin. Images are representative of at least three separate experiments. As a positive control for claudin-2, the expression of this protein in untreated Caco-2 monolayers is also shown. (B) Densitometric analyses of immunoblots of claudin-1, occludin (65 kDa) and high molecular mass (phosphorylated) occludin in the insoluble fraction of control and IFNγ-treated T84 monolayers. The graphs show the change in protein levels in IFNγ-treated monolayers as a % of control and are mean data from five separate experiments. Significant differences in protein levels were observed; *P<0.05; **P<0.01 compared with controls as indicated by paired t-test.
Studies were also undertaken to assess the reversibility of the functional and molecular changes induced by IFNγ. The IFNγ-induced decrease in TER was completely reversible such that 96 hours following IFNγ removal, TER values were not significantly different from untreated monolayers (Control: 1260±65; 96 hours post IFNγ: 1120±90 Ω.cm2; n=4). Similarly, the PEG permeability profile of T84 monolayers 96 hours after IFNγ washout were virtually identical to untreated monolayers although a consistent observation was that the permeability of the larger oligomers did not return fully to control levels (Fig. 7). As a result, whereas the 15-fold increase in β caused by IFNγ was largely reversed after 96 hours (Table 1), values remained slightly but significantly higher (P<0.05) than untreated controls. At the molecular level, the decreased expression of both 65 kDa and hyper-phosphorylated forms of occludin appeared to be completely reversed following removal of IFNγ for 96 hours (Fig. 8). However, the IFNγ-induced increase in claudin-1 in the insoluble fraction showed no evidence of reversal after 96 hours even though TER and PEG permeability had largely returned to control values by this time.
These data provide evidence that the pro-inflammatory cytokine, IFNγ does not mediate a general disruption of epithelial tight junctions but acts preferentially on a specific population of paracellular pores to increase the paracellular flux of compounds of higher molecular mass. The parallel effects of IFNγ on occludin phosphorylation provide preliminary evidence that this protein may be closely involved in regulating specific pore populations in the tight junction.
Reversibility of IFNγ induced alterations in paracellular permeability of PEG oligomers. Cells were treated with 10 ng/ml IFNγ for 48 hours. After this time IFNγ was removed from the medium and the cells were allowed to recover for 24 or 96 hours: ▪, no recovery; ○, 24 hours; •, 96 hours. A control profile (i.e. not exposed to IFNγ) is also shown □. Data are mean±s.e.m. of four monolayers in each group.
Reversibility of IFNγ induced alterations in paracellular permeability of PEG oligomers. Cells were treated with 10 ng/ml IFNγ for 48 hours. After this time IFNγ was removed from the medium and the cells were allowed to recover for 24 or 96 hours: ▪, no recovery; ○, 24 hours; •, 96 hours. A control profile (i.e. not exposed to IFNγ) is also shown □. Data are mean±s.e.m. of four monolayers in each group.
Discussion
Although single paracellular probes such as mannitol or high molecular mass dextrans are useful indicators of increased paracellular permeability caused by disruption of epithelial tight junctions, they do not offer the necessary resolution with which to analyse specific functional changes occurring in the paracellular pore. As a result, tight junction modulators are generally assumed to mediate their effects by simple dilatation of the junctional `pore' leading to a non-specific increase in paracellular permeability. The present study questions this assumption by using a functional profiling technique, which simultaneously measures the permeability of 24 PEG molecules of defined and increasing molecular size, to investigate the effects of the pro-inflammatory cytokine IFNγ on tight junctions in T84 cells. This technique resolves two different populations of paracellular `pores' in colonic epithelial monolayers, a population of restrictive pores with a radius of ∼4.5 Å (defined by α), which have a dominant role in the paracellular permeation of small molecules and a less abundant non-restrictive pathway (defined by β), responsible for the permeation of larger molecules (Watson et al., 2001). The present study provides evidence that IFNγ preferentially increases the permeability of larger molecules by modulating the non-restrictive pores (defined by β) in T84 cells while having little effect on the restrictive pathway either in terms of increasing the pore radius or the number of restrictive pores. Our hypothesis is that IFNγ activates specific pathways within the junctional complex that facilitate the paracellular passage of luminal macromolecules across the intestinal epithelium without a complete breakdown of the parcellular barrier to small solutes.
Reversibility of IFNγ effects on claudin-1 and occludin in T84 membranes fractions. T84 monolayers were treated for 48 hours with 10ng/ml IFNγ followed by removal of the cytokine for a further period of 96 hours as indicated and then extracted as described in Materials and Methods. Triton-soluble (S) and Triton-insoluble (I) fractions were immunoblotted with antibodies to claudin-1 and occludin. Images are representative of three separate experiments.
Reversibility of IFNγ effects on claudin-1 and occludin in T84 membranes fractions. T84 monolayers were treated for 48 hours with 10ng/ml IFNγ followed by removal of the cytokine for a further period of 96 hours as indicated and then extracted as described in Materials and Methods. Triton-soluble (S) and Triton-insoluble (I) fractions were immunoblotted with antibodies to claudin-1 and occludin. Images are representative of three separate experiments.
The molecular dimensions of the non-restrictive pathway cannot be estimated with the PEG oligomer series used here as the largest PEG oligomer (1250 kDa; hydrodynamic radius 7.4 Å) is smaller than other paracellular probes able to permeate across IFNγ-treated T84 cells. For example FD10 has a hydrodynamic radius of 23Å (Sanders et al., 1995). However, as the data in Fig. 2 demonstrates, there is a very close correlation between the IFNγ-mediated increase in FD10 permeability and IFNγ-mediated changes in the value of β, the descriptor of the non-restrictive pathway calculated from the PEG permeability profile. This supports the validity of using β to assess the contribution of this pathway to the permeation of large molecules following exposure to IFNγ. As noted previously (Watson et al., 2001), in unstimulated T84 monolayers the value of β is 15- to 20-fold lower than α indicating that under these conditions paracellular permeability is predominantly controlled by the restrictive pathway for small molecules. The dramatic (15-fold) rise in β on exposure to IFNγ suggests that the non-restrictive pathway will become a more significant component of junctional permeability in inflammatory conditions. This will have a proportionally greater impact on permeability to large compared to small molecules as evidenced by the relative increases in mannitol and FD10 permeation following treatment with 10 ng/ml IFNγ (fourfold for mannitol compared to 21-fold for FD10).
Although the limitations of conventional paracellular probes have limited investigation of functional heterogeneity in tight junctions, several observations are consistent with the current findings. Bijlsma and co-workers (Bijlsma et al., 1996) showed that carbachol increased the paracellular flux of horseradish peroxidase across isolated rat ileum to a much greater extent than small probes like mannitol. The authors hypothesised that this was due to the appearance of large diameter pores caused by fusion of smaller pores within the tight junction. Interestingly, freeze fracture studies of HT29-cl.19A cell monolayers showed discontinuities in tight junction strands after exposure to mixtures of IFNγ and tumour necrosis factor-α (TNFα), which was associated with a preferential increase in macromolecular flux (Rodriguez et al., 1995). Similar discontinuities have also been reported in the tight junctions of rat proximal tubule (Orci et al., 1981) and a dual-pathway model has recently been proposed for this tissue involving small tight junction pores (radius 6.7 Å) and infrequent large slit breaks (Guo et al., 2003), which is similar to that derived for colonocyte monolayers using the PEG profiling approach. Size-selective loosening of endothelial tight junctions has also been reported in claudin-5 deficient mice (Nitta et al., 2003) although, in contrast to the present studies, the effect appeared to be selective for small molecules of <0.8 kDa. Similarly, the differential effects of TNFα and the phorbol ester TPA on paracellular permeability in LLC-PK1 reported by Mullin and co-workers (Mullin et al., 1997) are also consistent with size-selective changes in junctional permeability. However, as neither of these studies analysed different size probes simultaneously, it is difficult to determine whether such effects involve activation of different pore populations or simply reflect the degree of dilation of the tight junction as a whole.
As previously hypothesised (Karczewski and Groot, 2000), the presence of multiple size- and charge-limiting pores within the tight junction offers potential for differential regulation of paracellular permeability by tight junction modulators. In previous studies, we have shown that EGTA and sodium caprate (C10) exert profoundly different effects on PEG profiling and sieving parameters in T84 cells (Watson et al., 2001). Exposure to C10 significantly increased the value of α but did not change restrictive pore radius, suggesting that its primary effect is to increase the number or open probability of restrictive pores. C10 did not significantly influence the non-restrictive pathway as evidenced by a lack of effect on β. EGTA, on the other hand, dramatically increased restrictive pore radius, abolishing all size discrimination and reverting the paracellular pathway in T84 cells to essentially a one-component system. The current studies demonstrate that the mechanism of action of IFNγ, which is to specifically influence the non-restrictive component of the pathway, is quite different and distinct from either of these modulators.
The molecular basis for different populations of paracellular pores and the mechanisms by which IFNγ modulates the non-restrictive pathway has not been specifically addressed in this study. However, the alterations in two tight junction proteins, occludin and claudin-1, which accompanied the IFNγ-mediated changes in permeability, suggest some potential avenues for investigation. Exposure to IFNγ markedly reduced the expression of occludin and its association with the detergent-insoluble membrane fraction, a finding that is consistent with other studies (Sugi et al., 2001; Mankertz et al., 2000; Oshima et al., 2001; Bruewer et al., 2003). Particularly noticeable was the loss of high molecular mass species, which reflects the phosphorylated form of the protein. The phosphorylation state of occludin appears to be an important regulator of paracellular permeability with several studies showing that dephosphorylation coincides with loss of TER and increased solute permeability (Simonovic et al., 2001; Chen et al., 2002; Ohtake et al., 2003). In the context of the present study, recent observations in the MDCK kidney epithelial cell line showing that knock down of occludin expression is associated with increases in tight junction permeability to large organic cations with little effect on mannitol permeability are interesting (Yu et al., 2005).
The increase in claudin-1 found in the detergent-insoluble fraction after IFNγ treatment is surprising because impairment of the paracellular route has generally been associated with reduced levels of this protein (Kucharzik et al., 2001; Tedelind et al., 2003), although recent reports of cytokine-induced increases in claudin-1 expression linked to barrier disruption indicate that this may not always be the case (Han et al., 2003; Abe et al., 2003). Interactions between claudins and occludin may be important in determining the properties of tight junction strands (Tsukita and Furuse, 2000; McCarthy et al., 2000). Given this, the possibility that an imbalance in claudin-1 and occludin caused by the divergent effects of IFNγ on these proteins could be involved in the formation of non-restrictive pores is worthy of consideration. Unlike the effects on occludin, the IFNγ-mediated increase in claudin-1 expression did not appear to be fully reversible and it is interesting in this respect that β values also remained significantly above control levels 96 hours after IFNγ washout suggesting that higher levels of the non-restrictive pore may persist after cytokine exposure.
It was important to exclude increased internalisation as an explanation for the selective increases in permeability of larger PEG and dextran molecules (7.4-23Å) induced by IFNγ. Both PEG and dextran are classical permeability probes being strongly hydrophilic molecules that are unlikely to diffuse across cell membranes to any significant extent, however, there is evidence that dextran, for example, may have a limited capacity to internalise via fluid-phase endocytosis. Shurety and co-workers (Shurety et al., 1998) demonstrated endocytic uptake of FITC-dextran in MDCK monolayers although the majority of uptake occurred from the basolateral surface with relatively little internalisation from the apical surface. Similarly, in T84, depletion of extracellular calcium has been shown to promote endocytosis of dextran (Ivanov et al., 2004), a finding which we have confirmed here. However, using the same approach, there was no evidence that IFNγ increased dextran internalisation over the small amount seen in untreated monolayers. This, taken together with the 14C-PEG4000 cell-association data, suggests that internalisation and transcellular passage of these paracellular markers plays no significant role in the selective modulation of permeability induced by IFNγ.
What is the relevance of these findings to the role of IFNγ in inflammatory disorders in the gut? Selective activation of a population of large pores within the paracellular pathway by IFNγ would allow large antigenic molecules to cross without gross disruption of the epithelial barrier to small molecules, which may occur at a later stage with the establishment of chronic inflammation. Increased exposure of the mucosal immune system to bacterially derived luminal antigens owing to impairment of the epithelial barrier is thought to initiate inflammatory responses (Linskens et al., 2001). IFNγ is increased in inflammatory conditions and has been shown to increase not only the paracellular movement of antigens but also their transcytosis across gut cells (Heyman, 2001). Selective activation of a population of large pores within the paracellular pathway by IFNγ would allow large antigenic molecules to cross without gross disruption of the epithelial barrier to small molecules, which may occur at a later stage with the establishment of chronic inflammation. Mucosal IFNγ levels have been shown to increase at an early stage in the development of colitis in mice (Spencer et al., 2002) and appear to rise very rapidly after oral antigen administration (Kolker et al., 2003). Although, the PEG profiling technique does not allow us to define the size of the IFNγ-stimulated pore, it would be expected to be large enough, based on the marked increase in FD10 permeability, to allow significant translocation of known bacterial antigens with molecular mass in the range 15-25 kDa (Yoshino et al., 1994; Orwin et al., 2002). The finding that IFNγ markedly increases T84 permeability to E. coli LPS supports this view, as although the precise molecular size of the LPS used here is unknown, purified LPS is thought to be in the region of 10-20 kDa. The routes and mechanisms by which LPS crosses the intestinal epithelium remains a controversial area. LPS can be internalised by gut epithelial cells via a clathrin- and lipid raft-dependent mechanism, a process which is involved in its intracellular recognition by toll-like receptor 4 (Hornef et al., 2003). However, the significance of this pathway in mediating increased transepithelial passage of endotoxin in disease states is unclear and recent studies (Drewe et al., 2001; Seth et al., 2004), including the present one, are consistent with enhanced permeability of LPS via a paracellular route in inflammatory or ischemic conditions. Interestingly, modulation of the tight junction by IFNγ does not however appear to be the primary route by which intact bacteria themselves cross the epithelium. Recent evidence from our laboratory has shown that IFNγ stimulates internalisation and translocation of commensal bacteria in gut epithelial cells via a raft-mediated transcellular process that appears to be independent of its effects on the paracellular pathway (Clark et al., 2005). The significance of the low levels of non-restrictive pathway detectable in unstimulated cells is unknown but may indicate a physiological, as well as pathological, role for the pathway. One possibility is that the pathway contributes to the low level sampling of luminal antigens necessary for development of immune tolerance, although there is evidence that this may also occur via a transcytotic route (Shao et al., 2001).
In conclusion, these studies suggest that proinflammatory cytokines may activate specific pathways within the tight junctions of intestinal epithelial cells that will favour the transepithelial transfer of large antigenic molecules. Although the significance of this pathway in vivo remains to be determined, the implication is that cytokines such as IFNγ may open up a paracellular route for the entry of luminal antigens without gross disruption of the epithelial barrier to small molecules. Such a pathway could be involved in the early pathogenesis of intestinal inflammatory disorders.
Acknowledgements
This work was supported by the Medical Research Council.




![Influence of IFNγ on mannitol and FD10 permeability across T84 monolayers. Following incubation with IFNγ-(0-10 ng/ml) for 48 hours, T84 monolayers were washed with HBSS and mounted in Ussing chambers. 100 μM [14C]mannitol or 10 μM FD10 (final concentrations) were added to the apical chamber and samples removed every 30 minutes for 3 hours for analysis of probe permeation. Results are shown as fold increase in permeability of mannitol and FD10 above control. Papp values for mannitol and FD10 in control monolayers were 0.53±0.15×10–6 and 0.015±0.005×10–6 cm/second respectively. Data are expressed as mean±s.e.m. of four monolayers in each group. Significant differences in permeability were observed; **P<0.01; *P<0.05 compared with control levels as indicated.](https://cob.silverchair-cdn.com/cob/content_public/journal/jcs/118/22/10.1242_jcs.02630/3/m_jcs02630f3.jpeg?Expires=1716284700&Signature=Dy9-Q6DdXlNMG3HG8q~Yp712fLDWE-9V89nk5iDWbStnyM-S6c3SzMalcoE997mlFKgvHYVTbKaC2lwRI04GQ5i7-ErxjY96g59Pp~58d6Fkfj8RNV9AA5NdKwtyyiifBkJUCFTaKf86viSDHe6Lx4v09z7rBcCxmz8Y~OOTVRvAUCwGwp7rcC9IkI27Qpu9L5lO~SqDidnfl9ntrvUj~Lr1pvILSqQFQg2tl-w8EKVIaBxPSk~xjNBuUYkBtJ0I70H299v-CjQ6adhC6b5aI76Gm5ncP918JyTFQ4hO4OYe~iAeqNh-KSbF6co1NDrOiMXXsymthVr9pUsnlnDNHg__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)