ABSTRACT
Little is known about how the initial endothelial plexus is remodelled into a mature and functioning vascular network. Studying postnatal remodelling of the retina vasculature, we show that a critical step in vascular maturation, namely pericyte recruitment, proceeds by outmigration of cells positive for α-smooth muscle actin from arterioles and that coverage of primary and smaller branches lags many days behind formation of the endothelial plexus. The transient existence of a pericyte-free endothelial plexus coincides temporally and spatially with the process of hyperoxia-induced vascular pruning, which is a mechanism for fine tuning of vascular density according to available oxygen. Acquisition of a pericyte coating marks the end of this plasticity window.
To substantiate that association with pericytes stabilizes the vasculature, endothelial-pericyte associations were disrupted by intraocular injection of PDGF-BB. Ectopic PDGF-BB caused the detachment of PDGF-β receptor-positive pericytes from newly coated vessels, presumably through interference with endogenous cues, but had no effect on mature vessels. Disruption of endothelial-pericyte associations resulted in excessive regression of vascular loops and abnormal remodelling. Conversely, intraocular injection of VEGF accelerated pericyte coverage of the preformed endothelial plexus, thereby revealing a novel function of this pleiotropic angiogenic growth factor. These findings also provide a cellular basis for clinical observations that vascular regression in premature neonates subjected to oxygen therapy [i.e. in retinopathy of prematurity] drops precipitously upon maturation of retina vessels and a mechanistic explanation to our previous findings that VEGF can rescue immature vessels from hyperoxia-induced regression.
INTRODUCTION
The formation of the vascular system is a complex process (for recent review see Risau, 1997). The initial endothelial plexus consists of a homogenous web of endothelial cell tubes and sacs, which later become remodelled into a mature network. Remodelling involves the creation of large and small vessels, the establishment of directional flow, the association with mural cells (pericytes and smooth muscle cells) and the adjustment of vascular density to meet the nutritional requirements of the surrounding tissue. Initially, the endothelial plexus is created in excess and the final adjustment of vascular density involves the regression of unnecessary vessels (i.e. vascular pruning). While much is known about factors and mechanisms that initiate vascular development, relatively little is known about the subsequent process of remodelling.
Several studies have suggested that association with mural cells is critical for proper vascular development and maintenance (for a recent review see Beck and D’Amore (1997) and Folkman and D’Amore (1996). Pericytes are cells surrounded by basement membrane and intimately associated with endothelial cells in the microvasculature (for review see Diaz Flores et al., 1991). Pericytes express alpha-smooth muscle actin (α-SMA) and thus have been implicated to have a contractile function. The origin of pericytes, however, is unclear. It has been suggested that pericytes are generated by in situ differentiation of mesenchymal precursors at the time of endothelial sprouting (Nehls et al., 1992). Other studies, using an ‘in vitro angiogenesis’ system have suggested that pericytes are formed by migration and de-differentiation of arterial smooth muscle cells (Nicosia and Villaschi, 1995).
In vitro studies have highlighted the possible role of pericytes and smooth muscle cells in regulating endothelial cell proliferation via secretion of inhibitory growth factors such as TGF-β (Orlidge and D’Amore, 1987) and inhibition of migration (Sato and Rifkin, 1989). Supporting data for the regulation of the endothelial cell network by pericytes is the observation that pericyte dropout precedes proliferative retinopathy in diabetic patients (Speiser et al., 1968).
A role for mural cells in maintaining vascular integrity was suggested by a number of gene knock-out studies. This includes disruption of the genes encoding the endothelial cell-specific receptors Tie1 and Tie2 (Dumont et al., 1994; Puri et al., 1995; Sato et al., 1995), the Tie-2 ligand, Angiopoetin-1 (Ang1) (Suri et al., 1996), Tissue Factor (TF) system (Carmeliet et al., 1996) and the Platelet-derived Growth Factor (PDGFB)/PDGF-β receptor system (Leveen et al., 1994; Lindahl et al., 1997; Soriano, 1994). Mice deficient in these genes show a hemorrhaging phenotype often associated with a reduced number of α-SMA-positive perivascular cells. ANG1- and TF-deficient mice also show defects in the remodelling of the homogenous yolk-sac vascular plexus. Lastly, a gain-of-function mutation in Tie2 has been implicated in the formation of venous malformation, characterized by vessels that are both abnormally large and have a deficient smooth muscle cell covering (Vikkula et al., 1996).
Both the analysis of knock-out phenotypes and in vitro studies, however, have not revealed the origin of mural cells, the dynamics of their recruitment and how pericytes effect vascular remodelling. To address these questions, a system to visualize and manipulate the developing vasculature in a natural, ongoing process is required. The retina vasculature is ideal for these experiments because of its unique architecture, its postnatal development in rodents and the possibility of molecular manipulation.
Earlier studies have highlighted the key role of oxygen in the formation and remodelling of the retina vasculature (for a recent review see Stone and Maslim, 1997). Briefly, as the retina increases in mass and neuronal activity is initiated, ‘physiological hypoxia’ is generated, VEGF expression is upregulated and acts to promotes vascular spreading across the retina. Exposure of a newborn rodent to 80% oxygen negates the increase in VEGF expression and leads to an underdeveloped retinal vasculature (Stone et al., 1995). In addition to preventing new vessel growth, hyperoxia leads to obliteration by apoptosis of already formed vessels. This suggest that vascular pruning that accompanies natural remodelling is caused by surplus oxygen delivered to the tissue upon the onset of flow through the newly formed system. Excessive vascular pruning is the initiating event in the pathogenesis of Retinopathy of Prematurity (ROP), a blindness-causing disease induced in premature infants placed in oxygen chambers. Using a rat model of ROP, we have shown that VEGF protects retinal vessels from hyperoxia-induced obliteration. These results suggested that VEGF (whose production is suppressed under hyperoxia) is required to sustain immature retinal vessels (Alon et al., 1995). It appears, therefore, that VEGF is critical for the survival of ‘immature/remodelling’ blood vessels and that independence from VEGF is a molecular hallmark of maturation. The unknown cellular and molecular basis of this maturation step is the focus of this study.
Here we provide a first evidence that the period of VEGF-dependence (i.e. immaturity) corresponds to a period in which new vessels are functioning but have not yet acquired a pericyte coating. We show that there is a developmentally programmed lag in the recruitment of pericytes to the preformed endothelial cell plexus and that this delay is essential in providing a plasticity window for the fine-tuning of the developing vasculature according to the nutritional needs of the retina. Findings reported here also uncover a function for VEGF in recruitment of pericytes, thus providing a mechanistic explanation for the protective role of VEGF against insults that initiate ROP pathogenesis.
MATERIALS AND METHODS
Immunohistochemistry of flat-mount retinas
Eyes from neonatal rats were fixed in 4% buffered formaldehyde. For dissection, the cornea, lens and sclera were removed, and hyloid vessels cleaned when necessary. Retinas were washed in PBS and permeabilized in 0.5% Triton/PBS for 2 hours. Primary antibody to α-smooth muscle actin, (SMA) (Sigma) and Bandeiraea simplicifolia BS-1 Isolectin (LEC) (Sigma) were added to 0.5% Triton/PBS/10% goat serum and incubated by shaking overnight at 4°C. Retinas were washed 4-5 times for 1 hour each with PBS. Secondary antibody anti-mouse FITC (for α-SMA) or extravidin-TRIC (for LEC) was added to 0.5% Triton/PBS/10% goat serum for 2 hours shaking at room temperature. Washing was repeated and retinas were mounted by making four incisions as shown in Fig. 1A. Retinas were mounted under coverslips and viewed either with conventional fluorescence microscopy or confocal fluorescent microscopy.
Schematic illustration of the retina vasculature. The retina is drawn to illustrate the alternating arrangement of arterioles (red) and venules (blue), the interconnecting capillaries and the three-dimensional organization of superficial and deep vascular plexuses. (A) Dissection along the dashed lines indicated is used to obtain a flat whole-mount preparation. (B) The superficial vascular plexus is overlying the ganglion cell layer (GCL) and will eventually remodel to form a less dense network with a range of vessel sizes and diameters. The lower plexus develops later by capillary descent followed by horizontal spreading between the inner nuclear layer (INL) and outer nuclear layer (ONL). (O) represents the optic disc.
Schematic illustration of the retina vasculature. The retina is drawn to illustrate the alternating arrangement of arterioles (red) and venules (blue), the interconnecting capillaries and the three-dimensional organization of superficial and deep vascular plexuses. (A) Dissection along the dashed lines indicated is used to obtain a flat whole-mount preparation. (B) The superficial vascular plexus is overlying the ganglion cell layer (GCL) and will eventually remodel to form a less dense network with a range of vessel sizes and diameters. The lower plexus develops later by capillary descent followed by horizontal spreading between the inner nuclear layer (INL) and outer nuclear layer (ONL). (O) represents the optic disc.
Microscopy
Conventional fluorescent and light microscopy was performed on a Zeiss Axioskop. Slide film was scanned into Adobe Photoshop 3.0 on a AGFA Arcus II scanner. Confocal microscopy was performed on a Zeiss Axiovert 135M outfitted with the software program LSM410. Double immunofluorescence with FITC and TRITC were visualized using filters BP510-525 and LP570. Images were printed from a CODONICS NP1600 Photographic Network Printer.
Injections into the vitreous of neonatal rats and hyperoxia exposure
Injection experiments always used one eye and the other was processed as a control. Mock injections of heat-inactivated growth factor and dilution buffers were performed many times to insure there was no phenotype on the vasculature due to injection. Each experiment was performed a minimum of 5-10 times and in several different injection sessions. Additionally animals of different ages were analyzed to see effects on various stages in vascular maturation. The left eye of each anesthetized animal was injected with 100 ng of recombinant growth factor in 1 μl sterile PBS. Injections into the vitreous humor were performed using glass capillary pipettes hooked to a micromanipulator. Animals were returned to mothers for 48 hours either in room air or 80% oxygen chambers.
In situ hybridization
Paraffin-embedded eyes from early postnatal rat pups were sectioned (5 μm thick), processed and hybridized in situ as previously described (Shweiki et al., 1992). Autoradiographic exposure was for 6 days. As a PDGF-β receptor-specific probe, we used a 1.5 kb fragment of mouse cDNA (kindly provided by Dr Battegay). cDNA were subcloned onto the polylinker of a PBS vector (Stratagene) and was linearized by digestion with the appropriate restriction endonuclease to allow synthesis of a 35S-labeled complementary RNA in the antisense orientation. RNA probe was fragmented by mild alkaline treatment prior to use for in situ hybridization.
RESULTS
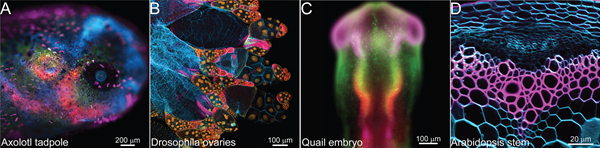
The rodent retina provides a unique opportunity to study all aspects of neovascularization and vessel remodelling since the course of vessel sprouting and assembly can be readily visualized using whole-mount retina preparations and specific immunostaining. Furthermore, the postnatal process is amenable to experimental manipulations via intravitreal injections (see below). Briefly, a superficial layer of vessels forms first, originating at the optic disc, spreading outwards radially as a homogeneous network of capillaries and reaching the edge of the retina in the second postnatal week. These vessels function to carry blood soon after their formation, even before remodelling into clear arterial and venous vessels is evident. In a second phase, a deep vascular plexus is formed by sprouting perpendicularly as far as the inner nuclear layer (INL) and extending branches parallel to the retinal surface (Fig. 1). Thus, in a retina aged between P1 and P18, a gradient of vascular development and subsequent remodelling can be traced between the optic disc and the retinal margin and between the superficial and deep networks.
Pericyte coverage takes place by outgrowth of arterial periendothelial cells and lags significantly behind vessel formation
Recruitment of mural cells to the endothelium is thought to be a key event in vessel maturation but it is unclear how pericytes become associated with the endothelium. Using a combination of an endothelial cell-specific marker Bandeira simplaficosia lectin (LEC) and a smooth muscle cell/pericyte-specific marker, α-smooth muscle actin (α-SMA), we show that α-SMA-positive cells are recruited to the preformed endothelial plexus by migration from the arterioles along the side branches in an arteriole-to-venule direction, leading to progressive coverage of first primary branches, and then of secondary and tertiary branches of the vascular tree. Consecutive stages in vessel remodelling are depicted in Fig. 2. Regarding the endothelial plexus (in red), the most pronounced remodelling event is a massive regression of capillaries, resulting in the formation of capillary-free zones (CFZ), around arterial vessels, and in a marked reduction in overall vascular density. For example, compare Fig. 2A and B, which show the same zone of the retina at postnatal days 2 and 10, respectively.
Acquisition of a pericyte coating by the preformed endothelial plexus. Double immunostaining of whole-mount retina with the endothelial cell-specific marker Bandeiraea simplicifolia lectin (red) and the smooth muscle cell/pericyte specific marker α-SMA (green). Confocal images are shown to visualize exclusively the superficial plexus or the deep plexus. (A) The superficial plexus at P2; (B) the superficial plexus at P10; (C) the superficial plexus at P18; (D) the deep plexus at P8; (E) the deep plexus at P10; (F,G) the deep plexus in the adult retina. To better illustrate the distribution of pericytes relative to that of endothelial cells, the red and green fluorescence were separated in the insets of A-C. a, arteriole. The following aspects of remodelling are notable: At P2, the capillary network is still dense, the capillary-free zone (CFZ) has not yet expanded and a thin layer of pericytes is found only on the major arterioles. The arrow points at a thinning branch on its way to be eliminated. At P10, the CFZ around arterioles has expanded and a CFZ start to form around primary branches which have also acquired a pericytes coating. The arrow points at a precapillary sphincter. At P18, both primary, secondary an tertiary branches from the arterioles are densely covered with α-SMA-positive cells. The lower endothelial plexus is still incomplete by day P8, it is completed by day P10, but still is pericyte-free. By adulthood, every vessel in the lower plexus (and, obviously in the upper plexus, not shown) is associated with α-SMA-positive pericytes. Scale bars reflect the relative magnifications in A and C.
Acquisition of a pericyte coating by the preformed endothelial plexus. Double immunostaining of whole-mount retina with the endothelial cell-specific marker Bandeiraea simplicifolia lectin (red) and the smooth muscle cell/pericyte specific marker α-SMA (green). Confocal images are shown to visualize exclusively the superficial plexus or the deep plexus. (A) The superficial plexus at P2; (B) the superficial plexus at P10; (C) the superficial plexus at P18; (D) the deep plexus at P8; (E) the deep plexus at P10; (F,G) the deep plexus in the adult retina. To better illustrate the distribution of pericytes relative to that of endothelial cells, the red and green fluorescence were separated in the insets of A-C. a, arteriole. The following aspects of remodelling are notable: At P2, the capillary network is still dense, the capillary-free zone (CFZ) has not yet expanded and a thin layer of pericytes is found only on the major arterioles. The arrow points at a thinning branch on its way to be eliminated. At P10, the CFZ around arterioles has expanded and a CFZ start to form around primary branches which have also acquired a pericytes coating. The arrow points at a precapillary sphincter. At P18, both primary, secondary an tertiary branches from the arterioles are densely covered with α-SMA-positive cells. The lower endothelial plexus is still incomplete by day P8, it is completed by day P10, but still is pericyte-free. By adulthood, every vessel in the lower plexus (and, obviously in the upper plexus, not shown) is associated with α-SMA-positive pericytes. Scale bars reflect the relative magnifications in A and C.
The acquisition of a pericyte coating (in green) lags significantly behind formation of the blood vessels. Thus, at day P2, while the endothelial plexus is already in place, only major arterioles are associated with α-SMA-positive cells (Fig. 2A). Outgrowth of pericytes starts with formation of precapillary sphincters composed of pericyte/smooth muscle cell clusters (arrow in Fig. 2B) and, by day 10, pericytes have spread out to cover only the primary branches (Fig. 2B). By day P18, pericytes have reached secondary and tertiary branches (Fig. 2C). Coverage of the deep plexus is even further delayed (Fig. 2D-G). Thus, none of the capillaries constituting the deep plexus is associated with pericytes at day P10 (although the deep endothelial network is already completed by that time) (Fig. 2E). The process of pericyte recruitment is only accomplished by adulthood (>3 weeks after birth) when all vessels in the deep plexus have acquired a pericyte coating (Fig. 2F,G). Importantly, there is no further remodelling of the endothelial plexus after the third postnatal week, neither with respect to changes in vessel diameter nor changes in vascular density. These observations, as well as a more detailed kinetic analysis (data not shown) have suggested that no further remodelling takes place after the acquisition of a pericyte coating.
Disruption of endothelial-pericyte interactions by ectopic PDGF-BB results in aberrant remodelling
It has recently been shown that PDGF-BB secreted by endothelial cells acts in a paracrine fashion to promote recruitment of pericytes expressing PDGF-β receptors (Lindahl et al., 1997). To show that PDGF-BB may play a role in recruitment of retinal pericytes, we performed an in situ hybridization analysis of retina sections with a PDGF-β receptor-specific probe. As shown in Fig. 3, pericytes are the predominant cells in the immature retina which express PDGF-β receptors, suggesting that pericytes are the likely target of PDGF-B, previously shown to be produced by retinal endothelial cells (Mudhar et al., 1993). We reasoned, therefore, that exogenous PDGF-BB added at the time of ongoing remodelling will interfere with the endogenous cues and, hence, would disrupt endothelial-pericytes interactions. Indeed, we show that intravitreal injection of PDGF-BB during the time of vessel remodelling resulted in disruption of endothelial-pericytes interactions and in formation of new aberrant EC-pericytes associations. Representative examples are shown in Fig. 4; precapillary sphincters, which function to regulate flow, are disrupted (compare the control eye in Fig. 4A with the PDGF-injected eye of the same animal in Fig. 4B). Elsewhere in the retina, instead of the usual tight wrapping around vessels, pericytes were associated with endothelial vessels in a disorganized fashion and often were connected to more than one vessel (Fig. 4C,D).
Expression of PDGF-β receptors by retinal pericytes. Retina sections of ages P7 (left) and P10 (right) were hybridized with a PDGF-β receptor-specific probe. PDGF-β receptor-positive cells (highlighted by arrows) were identified as pericytes on the basis of their periendothelial localization surrounding superficial vessels (left) and descending vessels (right). GC, ganglion cell layer ; INL, inner nuclear cell layer ; ONL, outer nuclear cell layer.
Expression of PDGF-β receptors by retinal pericytes. Retina sections of ages P7 (left) and P10 (right) were hybridized with a PDGF-β receptor-specific probe. PDGF-β receptor-positive cells (highlighted by arrows) were identified as pericytes on the basis of their periendothelial localization surrounding superficial vessels (left) and descending vessels (right). GC, ganglion cell layer ; INL, inner nuclear cell layer ; ONL, outer nuclear cell layer.
Disruption of pericyte-endothelial cells associations by ectopic PDGF-BB results in aberrant remodelling. (A) α-SMA staining demonstrates the normal structure of a P10 precapillary sphincter. (B) α-SMA staining of a PDGF-BB-injected P10 retina shows abnormal loosening of the endothelial-pericyte interaction and abnormal pericyte association with capillaries resulting in unusual branching structures. (C,D) α-SMA/LEC double staining of a PDGF-BB-injected P10 retina shows examples of pericytes completely dissociated from vessels and often in association with several vessels simultaneously. (E,F) Lectin staining of control (E) and injected eye (F) of the same P10 animal. The arrow highlights a broken vessel. PDGF-BB was injected 48 hours before removal of the retina. (G,H) The combined effect of hyperoxia and PDGF-BB is shown in a lectin-stained P10 retina following exposure to 80% oxygen for 48 hours either without (G) or with (H) injection of PDGF-BB prior to hyperoxic exposure. (I,J) The effects of ectopic PDGF-BB on the lower plexus is shown by lectin/α-SMA double staining of a P18 retina. Control (I) and PDGF-BB-injected eye (J) of the same animal are shown. For comparison, the superficial plexus of the PDGF-BB-injected eye is also shown (K and L for lectin and α-SMA, respectively). a, arteriole; v, venule.
Disruption of pericyte-endothelial cells associations by ectopic PDGF-BB results in aberrant remodelling. (A) α-SMA staining demonstrates the normal structure of a P10 precapillary sphincter. (B) α-SMA staining of a PDGF-BB-injected P10 retina shows abnormal loosening of the endothelial-pericyte interaction and abnormal pericyte association with capillaries resulting in unusual branching structures. (C,D) α-SMA/LEC double staining of a PDGF-BB-injected P10 retina shows examples of pericytes completely dissociated from vessels and often in association with several vessels simultaneously. (E,F) Lectin staining of control (E) and injected eye (F) of the same P10 animal. The arrow highlights a broken vessel. PDGF-BB was injected 48 hours before removal of the retina. (G,H) The combined effect of hyperoxia and PDGF-BB is shown in a lectin-stained P10 retina following exposure to 80% oxygen for 48 hours either without (G) or with (H) injection of PDGF-BB prior to hyperoxic exposure. (I,J) The effects of ectopic PDGF-BB on the lower plexus is shown by lectin/α-SMA double staining of a P18 retina. Control (I) and PDGF-BB-injected eye (J) of the same animal are shown. For comparison, the superficial plexus of the PDGF-BB-injected eye is also shown (K and L for lectin and α-SMA, respectively). a, arteriole; v, venule.
Disruption of normal endothelial-pericyte interactions had a profound effect on subsequent remodelling. The most reproducible phenotype was excessive breakage of capillaries followed by their obliteration, widening of the capillary-free zones and formation of irregular spaced vascular loops (compare the control eye in Fig. 4E with the PDGF-BB-injected eye of the same animal in Fig. 4F). A quantitative measure of vessel regression was obtained by sizing capillary-free zones (CPZ), using the LSM confocal software. Distances from the major arterioles to the first encountered secondary branch point in P10 retinas were compared between PDGFBB-injected eyes (n=130 branches) and uninjected eyes of the same animal (n=134 branches). This analysis showed that the CFZ was wider in treated eyes by an average 44%, with some regions showing even greater widening of the CPZ. Vessel breaking also led to the formation of capillary tangles, presumably due to abnormal tensile forces within the capillary network (Fig. 4).
As discussed above, the natural process of vascular pruning is induced by transient hyperoxia around the newly formed arterial vasculature and can be experimentally accelerated by subjecting neonatal pups to a oxygen-enriched atmosphere. This is recapitulated in Fig. 4 by comparing the much reduced vascular density in a P10 animal that has inspired 80% oxygen for 2 days (Fig. 4G) with its age-matched control (Fig. 4E). Injection of PDGF-BB before placing the pup in 80% oxygen aggravated the extent of vascular injury, more clearly revealing the abnormal remodelling seen by the uneven spacing of vascular loops and large areas devoid of microvessels (compare Fig. 4G, which is the uninjected eye, with Fig. 4H, which is the contralateral injected eye). These findings indicated that, in addition to abnormal morphology, disrupted endothelial-pericyte interactions render a newly formed vasculature more vulnerable to oxygen-induced vascular damage.
The effect of ectopic PDGF-BB on vascular remodelling was also examined with respect to the deep plexus. As in the superficial plexus, we observed that ectopic PDGF-BB disrupted the normal pattern of endothelial-pericyte associations and led to aberrant remodelling (compare the control eye in Fig. 4I with the PDGF-BB-injected eye in Fig. 4J). Interestingly, the difference in the developmental timing in which the superficial and deep plexuses are formed was reflected in the different timing in which PDGF-BB exerted the above effect. Thus, at the same time that ectopic PDGF-BB affected ongoing remodelling of the lower plexus (P18), it had no effect on the superficial plexus, which had already completed remodelling (Fig. 4K,L; the superficial plexus of the uninjected eye was shown in Fig. 2C).
VEGF rescues immature vessel from oxygen-induced obliteration by accelerating pericyte recruitment : implications for ROP
Exposure to hyperoxia is detrimental to the immature vasculature and leads to excessive regression of capillaries, primarily those branching from larger arterial vessels (i.e. those enjoying highest oxygen concentration). As vessels ‘mature’ they become refractory to this insult. This is illustrated in Fig. 5 showing that a 2-day exposure to hyperoxia leads to massive obliteration of capillaries if applied from P4-P6 (Fig. 5A) but has no effect if applied at a later age of P10-P13 (Fig. 5C). This animal model recapitulates the situation in the pathogenesis of retinopathy of prematurity (ROP) where therapeutic hyperoxia leads to obliteration of immature vessels in the retina of the premature infant but has no deleterious effect once the newborn has passed a critical gestation age.
Acceleration of pericyte recruitment by VEGF and rescue of immature vessels from oxygen-induced regression. (A,B) A P6 retina that has been exposed to 80% oxygen for 48 hours and stained for lectin (A) or α-SMA (B). Note that within the ‘cleared’ area, those vessels that survived are covered by pericytes (arrow). (C,D) A P13 retina that has been exposed to 80% oxygen for 72 hours and stained for lectin (C) or α-SMA (D). Note that at this stage hyperoxia did not cause obliteration of vessels. (E,F) Contralateral retina of the same animal shown in A and B except that VEGF was injected before exposure to hyperoxia. Note the full protection from hyperoxia-induced vessel regression (E) and an accelerated pericyte coverage (F). (G,H) P10 retinas of a pup raised in normoxia showing the extent of α-SMA staining in the left control eye (G) and 48 hours postinjection of VEGF to the right eye (H). Images are from the same region of the respective retina. a, arteriole; v, venule.
Acceleration of pericyte recruitment by VEGF and rescue of immature vessels from oxygen-induced regression. (A,B) A P6 retina that has been exposed to 80% oxygen for 48 hours and stained for lectin (A) or α-SMA (B). Note that within the ‘cleared’ area, those vessels that survived are covered by pericytes (arrow). (C,D) A P13 retina that has been exposed to 80% oxygen for 72 hours and stained for lectin (C) or α-SMA (D). Note that at this stage hyperoxia did not cause obliteration of vessels. (E,F) Contralateral retina of the same animal shown in A and B except that VEGF was injected before exposure to hyperoxia. Note the full protection from hyperoxia-induced vessel regression (E) and an accelerated pericyte coverage (F). (G,H) P10 retinas of a pup raised in normoxia showing the extent of α-SMA staining in the left control eye (G) and 48 hours postinjection of VEGF to the right eye (H). Images are from the same region of the respective retina. a, arteriole; v, venule.
A fundamental question is what marks vessel ‘maturation’ in the sense of becoming refractory to high oxygen. We examined the hypothesis that the determining factor is coverage by pericytes. Indeed, we found that within the most vulnerable fraction of retinal capillaries (i.e. primary branches from arterioles) those that survived hyperoxia are distinguished by the fact that they have already acquired a pericyte coating (Fig. 5B,D). In a previous study, we have shown that the molecular trigger of hyperoxia-induced vessel regression is downregulation of VEGF beyond the level required to sustain newly formed vessels (Alon et al., 1995). This result is reproduced here in the rescue experiment shown in Fig. 5E. Intravitreal injection of VEGF before exposure to hyperoxia completely prevented vessel regression (compare the VEGF-injected eye in Fig. 5E with the uninjected control eye in Fig. 5A, which is from the same animal). Unexpectedly, we found that injection of VEGF also accelerated the process of pericyte coating. Thus, whereas in the non-injected control only a few of the primary branches are covered by pericytes (Fig. 5B), in the VEGF-injected eye pericytes have spread further and have also covered secondary branches (Fig. 5F).
To confirm VEGF’s ability to enhance spreading of pericytes independently of hyperoxia, the effect of VEGF on pericyte spreading was examined under normoxic conditions. Again, injection of VEGF at a time where spreading of pericytes along the preformed endothelial network is just beginning resulted in marked acceleration of the process [compare the extent of pericyte coverage in the control eye (Fig. 5G) and the VEGF-injected eye (Fig. 5H) of the same animal]. The fields shown in Fig. 5G,H are from the edge of the retina, demonstrating that VEGF induces coverage of even the youngest vessels that, otherwise, would have acquired a pericyte coating several days later. These results revealed a novel function of VEGF, which is fundamentally different from its previously recognized roles as an endothelial cell mitogen, a chemoattractant or a permeability factor.
Interestingly, VEGF-treated retinal vessels appear wider than those in the control eyes (Fig. 5). To determine whether this is due to a thicker peri-endothelial coating or, alternatively, due to an increased lumen, both whole mounts and retina sections were stained with anti-α-SMA. As shown in Fig. 6, between postnatal days 7 and 15, there is an increase in the density of α-SMA-positive cells associated with the arteriole, however, without an increase in thickness of the peri-endothelial layer. Notably, VEGF did not change this situation. In contrast, VEGF induced endothelial cell proliferation, as judged by the detection of PCNA-positive cells in both superficial and deep plexus (assignment of PCNA-positive cells as mostly endothelial cells was aided by the fact that they are localized in the lining of large vessel in the superficial plexus and by the fact that pericytes have not yet entered the deeper layer at P10; Fig. 6E). Thus, we conclude that the increased width of the vessels in Figs 5F,H is primarily due to increased lumen diameter. Wider vessels have also been observed from VEGF overexpression in other systems (Benjamin and Keshet, 1997; Drake and Little, 1995).
VEGF-induced widening of vessels is due to increased endothelial proliferation. (A,B) A whole-mount preparation of P7 and P15 arterioles, respectively, showing an increase in density of associated α-SMA-positive cells. (C,D) Cross sections of control and VEGF-treated eyes, respectively, stained for α-SMA and visualized with peroxidase (red). (E) Detection of proliferating cells in a VEGF-injected P10 retina using an anti-PCNA antibody and peroxidase staining (black). The arrow points to a blood vessels in the superficial layer with several PCNA-positive endothelial cells.
VEGF-induced widening of vessels is due to increased endothelial proliferation. (A,B) A whole-mount preparation of P7 and P15 arterioles, respectively, showing an increase in density of associated α-SMA-positive cells. (C,D) Cross sections of control and VEGF-treated eyes, respectively, stained for α-SMA and visualized with peroxidase (red). (E) Detection of proliferating cells in a VEGF-injected P10 retina using an anti-PCNA antibody and peroxidase staining (black). The arrow points to a blood vessels in the superficial layer with several PCNA-positive endothelial cells.
DISCUSSION
Despite an increasing appreciation of the role that mural cells play in maturation, remodelling and maintenance of the vascular system, little is known regarding the process of their recruitment. It has been hypothesized that concomitant with sprouting, endothelial cells direct the differentiation of mural cell precursors from the adjacent tissue by the secretion of soluble factors (Beck and D’Amore, 1997; Nehls et al., 1992). A different view is that mural cells become associated with endothelial cells by migrating along newly made vascular sprouts (Nicosia and Villaschi, 1995). We find that pericyte coverage proceeds from the arterioles toward the venules, while vessel formation proceeds radially from the optic disc outwards. Coverage of primary and smaller branches takes place simultaneously along the arterioles, i.e. irrespective of the age of the vessel being covered. We support the view that pericytes migrate and proliferate along existing vessels (i.e. the arterioles to capillaries) at a developmentally programmed time.
Findings reported here provide a temporal framework for vessel maturation. Importantly, the recruitment of pericytes is significantly delayed and is lagging behind formation of the endothelial plexus by many days to a week. This finding suggests that, at least in the retina, pericytes are not likely to play a role in the initial formation of blood vessels. Instead, pericytes appear to influence the maturation and remodelling of vessels. The significant delay in periendothelial cell coating defines a transient stage of immaturity. We show that the time interval in which the vasculature is maintained without a pericyte coating coincides and, in fact, determines a window of plasticity for the vasculature to be remodelled and adjusted to the physiological needs of the tissue. In the retina, developmental remodelling of the vasculature mostly represents a feedback response to changes in available tissue oxygen. We propose that the natural process of vascular pruning represents an adjustment to surplus oxygen. The envisioned scenario is that developmental increase in retinal oxygen consumption and a resultant ‘physiological hypoxia’ is the driving force for VEGF-mediated neovascularization. However, only after the onset of flow through the newly made vasculature can the system be ‘checked’ with respect to the adequacy/surplus of oxygen reaching the tissue. Therefore, there is a physiological advantage to maintain the option of vascular pruning for a certain time after the formation of the initial plexus. We further argue that the end of the plasticity window, distinguished by the acquisition of a pericyte coating, prevents deleterious vessel regression due to transient fluctuations in tissue oxygen, which may occasionally take place in the mature animal.
A pathophysiological manifestation of this regulation occurs when premature infants are exposed to hyperoxia in order to compensate for immature lungs. Chronic exposure of the immature retina to hyperoxia leads to excessive pruning of the vasculature. When returned to room air, the remaining vasculature cannot supply the retina with sufficient oxygen and abnormal, excessive ischemia-induced neovascularization leads to development of ROP. The most critical factor in pathogenesis of ROP, recapitulated in our ROP rodent model, is the timing of the hyperoxic insult. Thus, the incidence of ROP drops precipitously when the premature baby is placed in hyperoxia at a late gestational age (Gibson et al., 1990) and does not develop in the rodent model if the insult is given later than 10 days after birth (Fig. 5). As shown here, the timing of acquiring immunity coincides with the timing of recruitment of periendothelial cells.
To establish a cause-effect relationship between pericyte coverage and resistance to ‘oxygen toxicity’, we used two experimental manipulations that either disrupt or accelerate natural pericyte recruitment. Disruption of endothelial cell-pericytes associations with ectopic PDGF-BB resulted in abnormal remodelling. Interestingly, we detected a differential sensitivity to ectopic PDGF-BB, suggesting that only pericytes engaged in ongoing migration were responsive. Once covered completely, the upper vasculature was unaffected by ectopic PDGF-BB, while the lower plexus was highly responsive. It seems likely that, just as the endothelial cells become mature, so do pericytes, at which point they no longer respond to earlier cues. A possible mechanism could be downregulation of PDGF receptors on retinal pericytes. Studies with PDGF-B-deficient mice have shown that PDGF is essential for proliferation and migration of pericytes along capillaries (Lindahl et al., 1997). Additional factors are likely to play a role in pericyte recruitment, including the Angiopoietin/Tie2 system, which appears critical for proper vascular maturity and integrity (Sato et al., 1995; Suri et al., 1996).
Just as disruption of pericyte-endothelial associations led to vessel regression, acceleration of pericyte recruitment by exogenous VEGF protected immature vessels from overpruning. VEGF appears to have three discrete roles in normal vascular development: it is capable of initiating angiogenesis via promoting endothelial cell proliferation and chemoattraction, it maintains viability of immature blood vessels and it facilitates the process of pericyte recruitment. Its role in accelerating pericyte coverage is a novel function, but the mechanism remains unknown. While it has been shown that VEGF receptors are expressed in cultured pericytes (Nomura et al., 1995; Takagi et al., 1996), it is possible that the observed effects of VEGF in vivo are indirect.
The finding that VEGF accelerated pericyte coverage also under normoxia argues against the possibility that increase pericyte covering in hyperoxia was simply due to increased vessel survival, since the vessels shown in Fig. 5G,H are in no danger of being eliminated either artificially or via normal remodelling. We have previously shown that VEGF is a survival factor for ‘immature’ vessels without understanding how VEGF prevented vessel regression. Based on our findings that VEGF accelerates pericyte coverage, and that only covered vessels survive hyperoxia, we propose that in hyperoxia exogenous VEGF rescues newly formed vessels partly by maintaining (and even facilitating) the normal process of pericyte recruitment.
Earlier work on VEGF-dependence of tumor vessels suggested that loss of VEGF led to detachment of endothelial cells from the vessel wall followed by their apoptosis (Benjamin and Keshet, 1997). This phenomenon of ‘anoikis’ resulting from the removal of a survival factor has been observed in other systems (for review, Meredith and Schwartz, 1997). It seems likely that VEGF is required in a positive way to maintain cell adhesion until periendothelial cells facilitate a more permanent mode of adhesion. We envision that newly formed vessels have a ‘provisional’ extracellular matrix (ECM) that allows for vessel plasticity. The mature ECM is likely composed of factors secreted by both endothelial cells and associated mural cells. It is known that newly formed and mature vessels express different integrin receptors. Specifically, the αV/β3 and αV/β5 integrins have been shown to be confined to angiogenic vessels in several systems including neovascularizing tumors and proliferative retinopathies (Brooks et al., 1994a,b; Friedlander et al., 1996). Reports of VEGF upregulating αV/β3 (Pepper et al., 1991) and the dependence of VEGF-driven angiogenesis on αV/β5 (Friedlander et al., 1995) support a possible link between VEGF-mediated survival and cell adhesion.
Finally, our findings provide a better rationale for preventing ROP through injection of VEGF prior to subjecting a premature infant to oxygen. Experiments in a rodent model of ROP have already shown that VEGF administered at this time may indeed protect retinal vessels from the hyperoxia-incurred damage (Alon et al., 1995).
ACKNOWLEDGEMENTS
We thank Ahuva Itin, Hadassa Gnessin, and Boaz Gilo for excellent technical help and Dr H. Spring (DKFZ, Heidelberg) for introducing us to confocal microscopy. This research was supported by the Israel Science Foundation (administered by the Israel Academy of Sciences) and by the foundation Mireille and James I. Levy, USA. L. E. B. was funded by the Valazzi-Pikovsky Fellowship Fund.